What is Diabetes?
Diabetes is a chronic disease that occurs when the body is unable to either sufficiently produce or properly use insulin. Insulin is a hormone secreted by the pancreas to help cells absorb sugar from the bloodstream and use it as an energy source.
When insulin is not adequately produced or properly used, it can result in elevated levels of blood sugar, called hyperglycemia. Hyperglycemia can cause deterioration of the body’s blood vessels, nerves and organs, most commonly the kidneys, eyes, and heart. Elevated blood sugars can leave a person more susceptible to slow healing wounds and infection, most commonly seen in the feet.
Type 1 diabetes is an autoimmune disease where the insulin producing cells of the pancreas are attacked, resulting in an insulin dependent body. It is also known as juvenile diabetes and is usually diagnosed in persons under 40, most commonly children. People that are diagnosed with Type 1 diabetes require an external source of insulin daily.
Type 2 diabetes is an acquired disease where the body does not produce enough insulin or does not properly use the insulin produced. It is most diagnosed in persons who are overweight or inactive physically, in individuals over 40 years old, but is now seen more in children and those under 40.
Type 2 diabetes can either be insulin or non insulin dependent based on the severity and chronicity of disease.
As of 2008-09, 2.4 million Canadians were living with diabetes. It is estimated that 90-95% of Canadians diagnosed with diabetes have Type 2 diabetes and 5-10% have Type 1.
How Does Diabetes Develop?

Diabetes development can be multi-factorial. There are many risk factors of type 2 diabetes, including inactive lifestyle, poor diet, family history, smoking, advanced age, or certain ethnicity.
Risk factors of Type 1 diabetes are currently not well understood, though there may be a genetic disposition or an environmental trigger that may initiate the autoimmune response.
Diabetes is normally diagnosed as either Type 1, or Type 2 and you cannot have both types of diabetes concurrently.
Hyperglycemia can be gradually increasing before onset of diabetes, and symptoms may go undetected. Diagnosis is usually made with a plasma glucose test. Hyperglycemic symptoms include; frequent urination, increased thirst, unexplained weight loss. Other symptoms can include blurred vision, fatigue, and nausea. Since these symptoms can be associated with other disorders or disease, diagnosis of diabetes may be delayed. It is best to control modifiable risk factors that may lead to diabetes: staying physically active, eating a healthy diet and eliminating smoking.
Why is Taking Care of my Feet Important?

Since diabetes can affect the blood vessels and nerves, the feet, situated the furthest from our nerve and vessel centre, are commonly affected in persons with long standing diabetes.
As other diabetes related complications can arise, the feet can become more affected and more difficult to manage. Complications include deteriorating eyesight, and decreased flexibility.
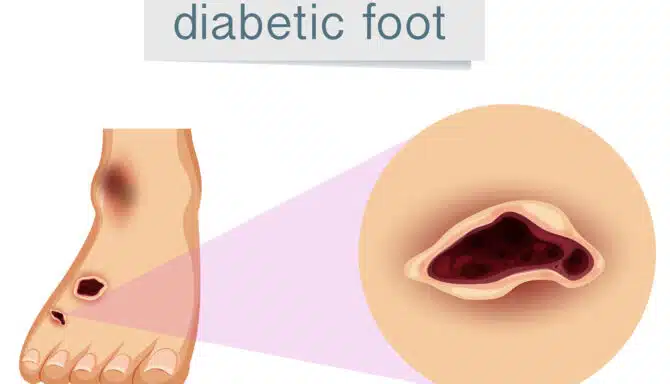
Decreased nerve function can reduce sensation in the feet, meaning small cuts and callus that may normally cause pain in a person without diabetes will go undetected. It is important to look at the feet regularly and immediately treat any developing callus or dryness to avoid foot wounds.
Decreased healing ability means infection may be a cause for concern in persons with diabetes. The feet generally see more sharp instruments than other areas including nail clippers, and files or blades to remove callus and corns and therefore are at higher risk for small cuts.
Taking care of feet in persons with diabetes are very simple and should become habit. The skin should be kept hydrated and elastic with use of cream and water consumption. All nails should be trimmed and filed to avoid any sharp corners. Avoid applying devices or items that are too hot or too cold directly to the skin.
Inspect the feet daily. If the feet are difficult to see, a mirror can be used. A friend or family member is the most helpful. The person should be looking for any of the following: increased redness, swelling, blood, foreign objects, callus, corns, dry skin, or deformity (bunion, hammertoe). If any signs are seen, visit a physician or book an appointment with one of our foot specialists.
A foot specialist is recommended for regular assessments every 6 months. If there are any concerns with the feet, regular foot care every month or 2 may be indicated.
Who Needs to Worry About Diabetes?
As of 2008, over 200 000 Canadians are diagnosed with diabetes every year. The increasing age of baby boomers and increased life span are contributing factors to the increase in diabetes diagnoses. The people most likely to be affected by diabetes are those in certain ethnic groups (first nations, African, Caribbean, south Asian and Hispanic), age groups (over 40), and higher weight groups.
In 2017, approximately 2.3 million Canadians (7.3% aged 12 and over) have been diagnosed with diabetes.
What Problems does Diabetes Cause for my Feet?
Diabetes can affect the feet in so many different ways: the skin becomes drier, the muscles start to change where foot deformities can develop, and the nerves are affected where sensation is reduced. Detection of problems can become difficult and due to decreased healing time and increased rates of infection; problems can progress rapidly.
Serious cases include undetected wounds, subsequent infection and possible amputation. Undetected wounds can paint a picture of uncontrolled diabetes, where multiple vital systems can be affected (kidneys, vessels, nervous)
At every age group, mortality rates are two times those in persons with diabetes than those without.
So, What Products Can I Use?
For persons with diabetes, it is important to avoid products with acid as an ingredient. Creams with mild acid solution can irritate the skin and cause small wounds.
Sharp objects such as nail clippers and foot files may be used in persons with controlled diabetes and with prior instruction from a professional. Feel free to use a daily cream and emollient to hydrate the skin.
Be careful using product between the toes, as that area can accumulate too much moisture which can breakdown the skin. Foot soaks can dehydrate the skin, please consult with your doctor or foot specialist before engaging in foot soaks.
Persons with diabetes may require shoes that are healthier for their sensitive feet. Shoes with soft foot beds that can reduce friction and increase shock absorption are ideal. Avoid shoes that have rigid seams or stiff out-soles.
When wearing shoes, keep an eye out for any red marks on the skin, these are ones to discard or avoid as they can one day leave a wound or laceration.
Will it Get Worse?
Persons with diabetes may feel their feet are too hot or too cold and try to use hot or cold packs to alleviate the discomfort. Due to decreased sensation, these hot/cold packs can cause hot or cold burns on the skin.
Be sure to protect the skin with a towel prior to using these types of warming/cooling packs, and test first on the hands as sensation is usually not as diminished in the hands. Never use hot water or hot packs – make sure the temperature is lukewarm.
If you have dry skin, make sure to moisturize; do not use harmful files or electric devices to remove callus or dry skin. Contact your chiropodist as you may be prescribed a cream. Inspect the feet daily, checking for cuts, callus or redness and swelling.
Where Can I Get Help? Who Can I Ask?
A licensed chiropodist is trained to treat feet, especially in those with diabetes. They can prescribe special creams, and carefully and safely reduce nail problems and callus. They can help reduce pressures by recommending orthopedic shoes or prescribing custom made orthotics.
They can improve mobility by offering specific exercises and stretches to keep you moving. And they are primary care practitioners who can monitor and inspect your feet for any new concerns.
Persons with diabetes should have a foot specialist examine their feet at least every 6 months. If you have callus or nail problems, a visit to the chiropodist can be a more routine visit at around 2 months. Regular examinations and visits can prevent foot complications that can occur with diabetes. Consult your doctor who can refer a foot specialist in your area or call our clinic today!