October 14, 2024
There are many at-home and natural remedies for foot pain that work, but there’s no denying the importance of foot exams with a top Toronto chiropodist. Some conditions require foot check-ups throughout the year and your foot clinic visits can make a big difference in not only your comfort levels, but your long-term health. Let’s take at what you can expect at a foot clinic appointment and why you should get your check-ups.
What You Can Expect at a Foot Clinic
This depends on if you’re visiting your foot clinic for the first time or are following up with a specific service, such as a custom orthotic casting and fitting or a medical pedicure.
At Toronto’s Feet First Clinic, your first foot check-up—an initial foot assessment—helps determine your unique needs. It’s your chance to discuss any concerns so your chiropodist can tailor the care to what matters most to you. Many people schedule one if they have persistent foot pain, but you may also do it for diagnostic purposes, footwear recommendations and more.
Why Schedule Regular Foot Check-ups?
Regular foot care is mandatory if you have diabetes. Studies show that neglecting your feet and failing to visit your foot specialist may lead to infections, ulceration and limb loss. While they sound extreme and scary, chiropody services can help you prevent these problems.
Chiropodist visits for diabetes include full examinations (particularly to assess for neuropathy), nail and skin care, wound debridement, and more. Some experts recommend coming in every 4-6 months, but this may be more or less, depending on your condition.
Foot check-ups are also a must for anyone with arthritis, circulatory issues, a history of strain injuries like plantar fasciitis, chronic fungal infections, to name a few. They’re especially important as we get older. But really, anyone can benefit from a little foot TLC—whether you're on your feet all day or just looking to prevent future problems, regular check-ups help keep your feet healthy, pain-free, and ready to go wherever life takes you!
An annual foot assessment is also a great preventative form of self care, like a wellness check for your feet. You don’t have to wait until you notice symptoms — assessments can catch early signs of the most common foot issues before they become painful.
August 5, 2024
Many people make it through their days without worrying about every little minor cut, scrape, ache or sensation. But for those with diabetes, foot care is a whole different ball game. Foot care for diabetes patients involves around-the-clock vigilance and solid diabetic foot care tips. These can prevent debilitating and life-altering diabetic foot complications, like severe mobility limitations, ulcers and even gangrene and limb loss. Let’s explore how a little goes a long way when it comes to foot health and diabetes.
Low-Impact Exercises and Stretches
Exercises and stretches that target diabetic neuropathy is one of the best strategies for protecting feet with diabetes.
To keep your feet as strong as possible, you need to stimulate blood flow and make sure nutrient-rich blood reaches your lower extremities. This can help wounds heal. Even if you have lost sensation in your feet, your muscles should still function properly enough to do light exercises.
Studies show that non-weight bearing and low-impact exercises and stretches can also improve motor score and help patients with activities of daily living (i.e.: basic chores, climbing stairs, etc).
To get started, check out the best exercises and stretches for diabetes.
Daily Inspections, Foot Hygiene and Nails
Preventing foot ulcers in diabetes patients involves frequently examining your own feet. A chiropodist should also do this for you, but more on that later!
Look at your feet multiple times per day. Are there any new wounds? Discolouration? Do your feet feel cold to the touch? Do you possibly have a fungal infection? Any abnormality should be noted.
Practice top-notch foot hygiene, as well. You can follow this general foot hygiene guide, but please note that diabetes patients are often advised not to cut their own toenails.
Schedule Regular Foot Assessments and Foot Care Services
At-home tips are great, but the truth is most diabetics need help managing foot issues. If you have diabetes, cutting your own toenails is often a bad idea because vision loss and neuropathy can cause you to not notice if you cut too deeply. Diabetes also affects the eyesight, so you may not notice any developing issues. And since diabetes causes circulation to the feet, these issues cannot properly heal. That's why one of the best services a chiropodist can perform is a medical pedicure that’s specially catered towards diabetes patients.
Your chiropodist can also:
Give advice on proper foot care. This often means investing in orthopedic footwear.
Provide wound care.
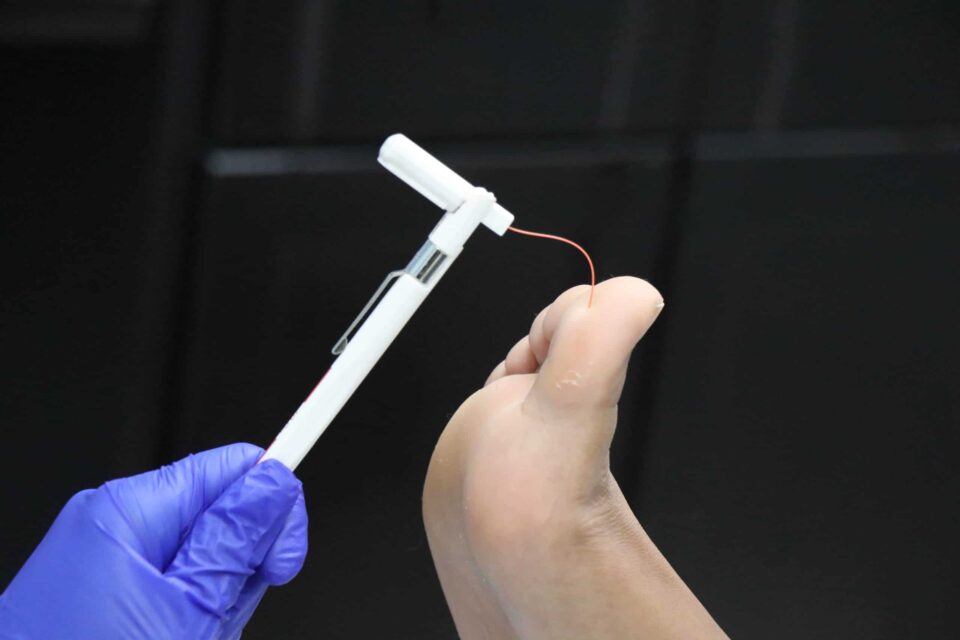
Assess for diabetic neuropathy — how severe is it?
Assess your blood circulation.
Inspect for potential ulcers.
If you live in the Greater Toronto Area, one of our Toronto chiropodists can perform routine diabetic foot care and diabetic foot assessments to help prevent diabetic foot complications. Click here to learn more about our foot care services for diabetes patients.
Additional Diabetic Foot Care Tips
Never go barefoot, even at home. Wear house shoes or orthopedic slippers. Being barefoot is too risky for diabetes patients, as if you stub your toe or cut yourself, the wound can't properly heal.
Avoid direct heat sources, like a really hot foot bath. It can dry out your skin and make your feet more susceptible to cracking.
Consider custom orthotics by learning when you might need them.
June 10, 2024
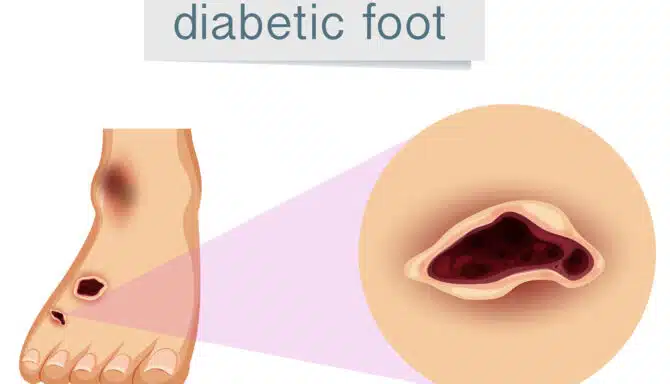
Not fully understanding of diabetes complications and the importance of preventative diabetic foot care can be detrimental. Diabetic ulcers (sometimes called diabetic foot) often occur after the onset of diabetic neuropathy, which severely restricts sensation in the feet. Around 40-50% of diabetes patients develop neuropathy; people with type 1 diabetes may develop it years after their diagnosis, while those with type 2 can sometimes already have neuropathy in the pre-diabetes stage.
Today, we’ll explore how minor cuts and scrapes, combined with neuropathy, can lead to ulcers and progressively severe issues. But with solid diabetes awareness and preventative measures, serious complications can be easily avoided!
How Cuts and Scrapes Turn Into Diabetic Ulcers
Here are the five stages between a tiny wound and a full blown diabetic ulcer:
Stage 1: Initial Injury
A minor injury such as a cut or scrape occurs on the skin — anything from a small burn to stepping on a piece of glass. Foot conditions that open the skin’s barrier can also cause tiny wounds, like blisters, cracked heels, calluses and ingrown toenails. For individuals without diabetes, these usually heal without complications.
Stage 2: Diabetes Impairs Circulation and Wound Healing
Diabetes and diabetic neuropathy halts the wound healing process, especially if diabetes is uncontrolled. First, high blood sugar levels harm blood vessels and restrict the oxygen-rich blood flow our injuries need for repair. Neuropathy also causes a loss of sensation, meaning you may not even be aware of the cut or scrape.
Stage 3: Infection
The wound may become red, swollen, and warm, indicating infection. Pus or an unusual discharge might be present.
Stage 4: Chronic Wound
The cut or scrape evolves into a chronic wound, characterized by persistent inflammation and failure to heal after several weeks.
Stage 5: Diabetic Ulcer
An ulcer forms as an open red or pink sore that looks “punched out.” It may penetrate deeper layers of skin, extending to muscle or bone in severe cases. Tissue death (necrosis) can also occur, leading to blackened areas around the ulcer. Ulcers can lead to extensive tissue death (gangrene) and bone infections when ignored.
What You Can Do to Prevent Diabetic Ulcers
Ulcers sound scary, but the good news is that being vigilant about your foot health can help keep your feet ulcer-free. Examine your feet at home every day, keep them clean, and wear protective orthopedic slippers while inside to protect your skin. Lastly, you should regularly visit your chiropodist for inspections and diabetic foot care if you have diabetes; ask them how frequently you should be coming in!
March 28, 2024
Wondering about top foot moisturizing tips and dry skin remedies? Look no further! Skin-related issues are common at Feet First Clinic, so we know a thing or two about the secrets behind soft feet! Keep reading to master our step-by-step guide on the perfect hydrated skin care routine for your feet.
Foot Moisturizing Tips: A Step-by-Step Guide
Numerous studies support the use of high-quality moisturizing creams on the feet to fight xerosis (the medical term for dry skin).
Dry skin acts as a foundation for common foot problems, like pain and soreness, bleeding, cracked heels, peeling skin, and more, so moisturization not only makes your feet feel smooth to the touch, but it also gives you protection against future troubles. Moisturizing can also help you manage more serious concerns, like diabetes and psoriatic arthritis.
Below are the steps you should follow to guarantee you are lathering your feet up the right way:
Step 1: Get the right products
Step 2: Cleanse and exfoliate your feet
Step 3: Moisturize your feet
Step 4: Protect and maintain
Step 1: Get the Right Products
For the best results, choose medicinal moisturizing creams from brands like Gehwol. These focus on hydration, are fragrance-free and made without harsh chemicals.
Their Soft Feet Cream contains urea (which absorbs moisture and softens skin) and glycerin (which relieves dryness and retains moisture). It also contains soothing and pleasant ingredients like avocado oil and honey extract.
Their Med Salve for Cracked Skin may be the best bet for a more aggressive moisturizing treatment. Due to it being a salve and not a cream, it is specially designed to penetrate the skin more thoroughly. Likewise, in addition to being a good choice for people prone to cracked heels, it is suitable for diabetics. Another good option is the deep penetrating heel care cream from Dermal Therapy.
Step 2: Cleanse and Exfoliate Your Feet
Before moisturizing comes foot hygiene! You should always start with a clean base. Clean your feet in warm water with fragrance-free, gentle soaps, and thoroughly dry, especially in between the toes (vulnerable area for fungal infections). To go the extra mile, exfoliate your feet with a scrub product and finish off with a foot file on the bottom of the feet. This eliminates dead skin cells, making your moisturizer more effective!
Step 3: Moisturize Your Feet
Moisturizing itself is pretty simple. Use a generous dollop (but not too much) of moisturizer and focus on dry areas, if you have any. Massage the moisturizer into your feet using circular motions, ensuring full coverage. Avoid the area in between the toes if you’re prone to infections or wounds (if you have diabetes). Moisture can build in the between the toes more easily than other areas.
Step 4: Protect and Maintain
Repeat this process regularly, ideally daily or at least a few times a week, to keep your feet soft, smooth, and well-hydrated. If your skin is especially vulnerable and sensitive, like for those with psoriasis and psoriatic arthritis, a regular routine is extra important to help you manage painful flar- ups.
March 7, 2024
Foot health directly correlates with our overall wellness. Seniors, in particular, can learn a lot about their general health when they start to understand the biomechanics of healthy feet. How feet look, how they feel, and how they function can be a sign of a serious health issue. This is also true in reverse — neglecting foot health can lead to conditions and other problems. Let’s take a look at how our feet act as a mirror to our holistic health. Here are the two main topics we'll break down today:
How our feet can signify poor health
How neglecting foot health affects overall wellness
How Our Feet Can Signify Poor Health
Your feet will often try to warn you that you need to visit your family doctor or foot specialist. Some of these warning signs include:
Cold feet
Feet that are cold to the touch and don’t seem to warm up can be a sign of a blood circulation or heart issue. Icy cold feet can also be a sign of peripheral artery disease, which is the narrowing or blockage of blood vessels in the lower extremities, or a thyroid condition.
Sores and wounds that don’t heal
Diabetes is arguably the medical condition most notorious for damaging our feet. Elevated blood sugar levels can make our feet more susceptible to wounds. Even the tiniest blister, cut, or callus that doesn’t bother the average person can become a major concern. Wounds that do not heal can become infected and lead to devastating problems like gangrene and amputation.
Numbness and tingling
Bizarre foot sensations are also often a tell-tale sign of diabetes. They warn us that diabetes has progressed to the point of neuropathy (when the disease causes nerve damage).
Foot swelling (edema)
Injuries, medications, heart and kidney problems, and more can all cause fluid to accumulate in the tissues. Edema can also be a sign that you need to eat less salty foods.
Foot pain
From plantar fasciitis to Morton’s neuroma, painful feet can be a sign of many conditions, and it’s tough to really narrow down the cause. Sometimes it may be from simply ignoring foot care for years (wearing unsupportive shoes, not using inserts or orthotics, etc), but sometimes it may be a sign of age-related joint deterioration, like osteoarthritis, or weight gain.
Strange colouring
Toes that turn red, white or blue may be a sign of Raynaud’s disease (this can also make your feet very cold). This condition often causes blood vessel “spasms” due to their narrowing, and may be connected to stress and cold weather.
How Poor Foot Health Affects Overall Wellness
Taking care of your feet plays an imperative role in an overall healthy lifestyle. Everyone should practice foot care, but foot health tips for seniors are extra important as we age.
Outside of foot pain and the common foot conditions we all know about, here are some other ways poor foot health can affect you:
Back, knee and hip pain
Foot issues may contribute to pain and discomfort in the back, knees, and hips due to altered gait and poor posture. This happens when you adopt unusual walking patterns to make up for the fact that your normal stride is painful. Remember, the musculoskeletal system is all connected!
Heightened injury risk
Weaker feet = more likely to fall and do some serious damage. Ignoring things like strengthening exercises and wearing proper footwear can lead to vulnerable feet.
Infections
Don’t ignore skin and toenail issues and assume they will magically go away! We already touched on how important this is for diabetes patients, but brushing off problems like fungal conditions can lead to painful infections that may even harm your immune system. This is true for everybody.
February 8, 2024
As the golden years unfold, maintaining an active and pain-free lifestyle should be a priority for seniors. One often overlooked aspect of overall well-being is foot health.
Our feet, the unsung heroes of a lifetime of steps, require special attention to ensure comfort and mobility. This article delves into practical foot care tips for seniors, empowering you to stride into each day pain-free and with a zest for life.
Choose supportive footwear
The foundation of pain-free feet lies in the shoes we wear. Opt for supportive footwear with cushioning, proper arch support, and a comfortable fit. Also consider wearing supportive footwear indoors to provide support and protect against slips and falls on slippery surfaces.
Read our complete guide to senior foot care in this blog post.
Regular foot inspections
Make it a habit to inspect your feet regularly. Look for any changes in colour, swelling, or unusual growth. Recognizing early signs of issues can prevent more significant problems, ensuring your feet remain a source of strength - not pain.
Gentle foot exercises
Keep those joints and muscles limber with gentle foot exercises. To do this, add lower leg exercises to your daily routine to maintain and improve mobility. Exercises like ankle circles, toe flexes, and heel lifts can improve flexibility and strength, promoting pain-free movement.
Moisturize and combat dry skin
Seniors often contend with drier skin, leading to cracks and discomfort. Combat this by moisturizing your feet regularly, paying particular attention to the heels and soles; Well-hydrated skin is more resilient and less prone to issues. You may also consider regular foot care appointments with a chiropodist, who specialize in senior foot care.
Elevate your feet to reduce swelling
After a day of activity, give your feet a break. Elevate them when resting to reduce swelling and promote healthy blood circulation. This simple practice can significantly affect how your feet feel after a busy day.
Address foot pain promptly
Don't ignore foot pain or discomfort. Consult with a chiropodist or healthcare professional to address any issues promptly. Early addressing can help combat the development of chronic conditions and ensure that your feet remain pain-free. Consider an annual foot assessment for a comprehensive check-up on the health of your feet. Studies show that physical examination of the feet as part of the routine assessment of older adults is imperative to detect foot problems. A foot assessment includes:
Circulation and blood flow to your feet
Neurological status
Changes or concerns with the skin and toenails
Your foot type (i.e., flat feet, normal arches or high arches)
Biomechanical abnormalities (i.e. limited or excessive range of motion in joints, areas of pain, overpronation, etc.)
Low-impact exercises for overall health
Staying active is vital to a vibrant lifestyle. Engage in low-impact exercises like walking, swimming, or tai chi to promote cardiovascular health without putting excessive strain on your feet and joints.
Custom orthopedic inserts
Enhance comfort and support by considering custom orthopedic inserts for your shoes. These inserts provide additional cushioning and support for your arches, reducing the risk of foot-related discomfort.
Prioritize circulation
Good circulation - the rate at which your blood flows to and from various body parts - is vital for overall foot health. Avoid prolonged periods of sitting or standing, and consider simple exercises to promote blood circulation. Compression stockings can also benefit you by improving your blood circulation. Your feet will thank you for the improved oxygen and nutrient supply.
Maintain a holistic approach to health
Remember that foot health is interconnected with your overall well-being. Maintain a balanced diet, manage your weight, and stay hydrated. A healthy lifestyle reflects positively on your feet and contributes to your ability to stay active.