July 25, 2024
Foot pain can be debilitating, affecting our ability to walk, exercise, and perform daily activities comfortably. One common foot condition that causes discomfort and requires attention is crossover toe.
This blog post delves into crossover toe, its symptoms, and available treatment options. First off, we'll explain exactly what is a crossover toe.
What is a crossover toe?
Crossover toe, also known as floating toe or floating fifth toe, is a type of deformity in which the toe drifts out of its normal position and crosses over or under a neighbouring toe. The condition is also known as overlapping toe.
The condition generally affects the fourth and fifth toes, leading to pain, swelling, and difficulty wearing shoes comfortably. However, any combination of toes may become an overlapping toe. Roughly 7% of adults—men and women equally — have overlapping toes of some sort.
Symptoms of crossover toe
Toe pain: Discomfort is often felt at the base of the affected toe, especially when walking or standing for long periods.
Swelling and inflammation: The affected area may become swollen and inflamed due to the abnormal positioning of the toe.
Uncomfortable shoe fit: Shoes may feel tight or uncomfortable, especially in the toe box area where the affected toe rubs against adjacent toes or the shoe itself.
Visual appearance: The affected toe may appear to cross over or under the adjacent toe, giving it a visibly different appearance than the other toes.
Corns: Corns will often form on top of crossover toes due to excessive friction and rubbing on the affected toes.
Causes of crossover toe
Crossover toe can develop due to several factors, including:
Foot injuries: Joint and ligament damage caused by unhealed trauma and foot injuries can change the toes' alignment over time. Additionally, arthritis, including rheumatoid arthritis, can shift the alignment of your toes as it progresses and damages the joints.
Foot structure: People with high arches or flat feet are prone to developing overlapping toes.
Genetics: Overlapping toes may also be inherited. Many conditions that make one prone to developing an overlapping toe, like arthritis and Morton's toe, have genetic contributing factors.
Improper footwear. Wearing shoes that are too short, too narrow or too tight can force the toes into an unnatural position and curl up, which will ultimately lead to the development of a crossover toe.
Treatment options for crossover toe
Footwear adjustments: Proper-fitting footwear is one of the most important ways to manage a crossover toe. Switching to shoes with a wider toe box can ease pressure on the affected toe and reduce discomfort. You should also make sure you have sufficient space at the end of your shoes (typically 1 cm) for your toes to properly splay. If shoes are too short, your toes will curl up. Many companies, like ASICS, APEX and Saucony, offer a wide-width options to give your feet the extra room it needs. Shoes with a mesh or soft upper are also recommended, as this will reduce pressure and friction on the top of the toes.
Orthotics Custom orthotic inserts or pads can help support the arch and redistribute pressure across the foot. This can help promote proper toe alignment and reduce pressure on the crossover toes so that they don't get worse.
Foot and Toe exercises: Performing specific exercises to strengthen the muscles and tendons around the toes can improve flexibility and prevent the condition from progressing.
Splinting or taping: A foot specialist can tape the affected toe to encourage proper alignment and reduce pain. You can also buy a splint or toe spacer to help stabilize and align the toe.
Corn and Callus Treatment: Since crossover toes are extremely prone to corns and calluses, it is very important to see a licensed chiropodist for routine foot care. A chiropodist can safely debride any corns and calluses on your crossover toe, which will reduce pain and irritation.
July 18, 2024
Feet come in all shapes and sizes, and while many people have heard of common foot conditions like bunions or flat feet, there's another lesser-known but equally interesting foot characteristic called Morton's foot or Morton's toe.
The condition occurs when the second toe is longer than the big toe, leading to potential biomechanical implications and foot-related issues. Let's delve into Morton's Foot, its potential effects on foot health, and how to manage it.
What is Morton's foot/toe?
Morton's Foot, also known as Morton's toe/foot or Greek foot, is a foot structure in which the second toe is longer than the big toe. The big toe is the longest in a typical foot, followed by the second toe. (Despite sharing the same name, Morton's neuroma and Morton's toe are not the same.)
However, in individuals with Morton's foot, the second toe extends beyond the big toe, sometimes significantly. The condition is quite common. As many as 40%+ individuals have a longer second toe than a big toe.
Potential biomechanical implications
But here's the twist: while Morton's foot is generally considered a variation of normal foot anatomy rather than a medical condition, it can have some surprising biomechanical implications that affect gait and foot function. Let's explore these potential issues associated with Morton's foot.
Added pressure on the second toe
The longer second toe may bear more weight during walking or standing, leading to increased pressure and potential discomfort or pain in the ball of the foot, which may contribute to clawing of the toe and hammertoes.
Gait changes
Morton's foot can alter the distribution of weight and pressure across the foot, potentially affecting gait mechanics and posture. This may contribute to overpronation, increasing the risk of injuries such as plantar fasciitis, shin splints and bunions.
Footwear challenges
Finding the right footwear can be a real challenge for individuals with Morton's foot. Shoes often fail to comfortably accommodate the longer second toe, leading to issues such as rubbing, irritation, or the development of thickened or ingrown toenails, corns or calluses on the affected toe.
How to manage Morton's foot
While Morton's Foot may not require medical intervention, there are steps individuals can take to manage associated discomfort or mitigate potential issues proactively:
Choose footwear wisely. Opt for shoes with a wide toe box to comfortably accommodate the longer second toe—Asics is a great choice for a roomier and wider toe box. Avoid narrow or pointed shoes that can squeeze or crowd the toes.
Consider orthotic support. Custom orthotic inserts or insoles can offset pressure on the toes and support the foot. This can alleviate any discomfort associated with Morton's Foot and improve your overall foot mechanics.
Foot-strengthening exercises. Engaging in exercises to strengthen the muscles of the foot and ankle can help improve stability and support, reducing the risk of overuse injuries or discomfort associated with Morton's foot.
Regular foot care. Practicing good foot hygiene and monitoring for signs of irritation or injury can help prevent complications such as corns, calluses, or ingrown toenails on the longer second toe.
July 15, 2024
Just like the rest of your body, your feet change with age. There are many age-related foot conditions that can target anyone at any time, but are more likely to occur in our golden years. With proper care, foot health in older adults doesn’t have to be too challenging and your aging feet can step out in downtown Toronto with confidence (and more importantly, in comfort).
Why Aging Feet Become Vulnerable
Studies show that one of the reasons musculoskeletal foot conditions, toe deformities and ankle problems are more common in older adults aged 65-74 is due to ill-fitting footwear.
Poorly fitted shoes not only wreak havoc on your feet, but if you’ve worn them for double the amount of years a younger adult has, then they’ve had more time to cause foot issues! The math speaks volumes and is one of the many reasons wearing good shoes from a young age is so important.
A change in size and shape also signifies your feet are getting older. Your body’s ligaments and tendons lose their ability to “spring back” which causes fallen arches (flat feet). This also relates back to ill-fitting footwear; if you aren’t aware of your foot changes, you can wear shoes that are too small without realizing it.
Your skin also becomes thinner when you get older, and your nails more brittle and fragile. Your toenails can also get thicker, but not in a healthy way. Their weakening can invite unwanted problems like fungal infections and skin conditions.
Lastly, it's only natural for a little wear and tear to set in after years of walking on your feet - after all, we only get one pair! This can cause degradation in many of the 33 joints in the foot.
Common Foot Ailments In Elderly People:
Bunions
Hammertoes
Plantar fasciitis
Osteoarthritis
Gout
Type 2 diabetes and diabetic neuropathy (commonly occurs after age 45)
Calluses
Corns
Toenail fungus
Elderly-onset rheumatoid arthritis (a different type of RA than the one that targets younger adults)
Foot Care Tips and Footwear For Seniors
Managing foot problems and caring for aging feet is achievable when you do the following:
Wear shoes that fit well! Many foot conditions feel better and more manageable when you wear orthopedic shoes, shoes for sensitive feet or the best shoes for seniors.
Also, find shoes with the right level of shock absorption to protect your joints.
Consider custom orthotics.
Perform regular, low-impact exercises and stretches to keep your feet strong and flexible. Yoga and swimming is a great idea, but there are also exercises for arthritis.
Keep your feet clean and moisturized.
Get medical pedicures to maintain your nail health.
Manage conditions like gout with proper dietary health and learn the role of nutrition in foot health.
Try other products and medical devices like bunion pads, correctors, etc.
Learn more about age-defying foot care.
June 6, 2024
Our feet and toes change in various ways as we age. One of these changes is toenail thickening.
For some of us, toenail thickening can be more than just a minor inconvenience. It can make it difficult to cut and maintain our toenails, and can even cause pain and discomfort. In this article, we'll explain the causes of thickened toenails, and some possible treatments.
Why Do Toenails Thicken with Age?
Nails are made from a protein called keratin, which is produced at the nail plate at the base of the nail. Nail growth happens when nail cells multiply within the base of the nail and are pushed forward. However, as we age, the growth rate slows down, so the nail cells just pile up on top of each other, which causes them to get increasingly thicker.
Toenail thickening is often a result of several factors:
Reduced blood circulation
The most common cause of toenail thickening is decreased blood circulation to our feet. This diminished circulation means fewer nutrients and oxygen reach the toenails, causing them to thicken over time. Age is one of the risk factor for reduced blood circulation to the feet.
Natural wear and tear
Years of use can damage our toenails. Factors such as ill-fitting shoes, repetitive stress from activities like running or walking, and even minor trauma can contribute to thickening. Essentially, when our toenails experience trauma, they thicken to protect themselves. As we age, wear and tear on our toenails can accumulate, which can cause them to thicken.
Fungal infections
Older individuals are more prone to fungal infections of the toenails, which can cause thickening, discoloration, and brittleness. These infections often thrive in warm, moist environments like sweaty shoes or communal areas.
Underlying health conditions
Medical conditions like psoriasis, diabetes, and peripheral arterial disease can also influence toenail health. These conditions affect circulation, which in turn slows toenail growth and causes toenails to thicken.
Tips for toenail care as you age
As you age, proactive steps can be taken to maintain healthy toenails and minimize thickening. By following these tips, you can feel more in control of your foot health and well-being.
Regular trimming
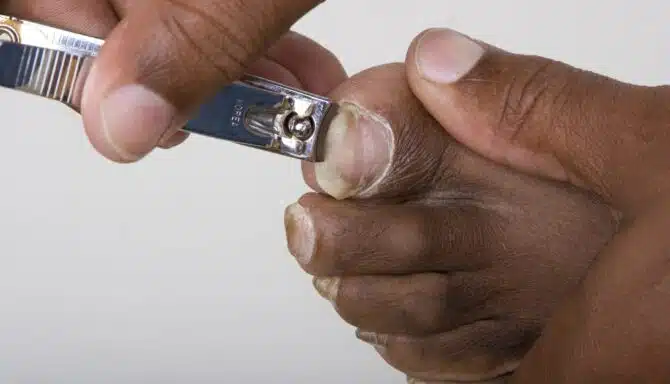
Toenail thickening can make trimming and maintaining your toenails extremely difficult. Fortunately, a licensed chiropodist is trained to specifically deal with this. A licensed chiropodist can ensure your toenails are trimmed properly to prevent ingrown toenails, promote healthy toenail growth and reduce thickening. A licensed chiropodist can also use special tools over the toenail to thin it out, which will make the toenail easier to cut and maintain. Best of all, this is all done in a sterilized environment, so you don't need to worry about fungal infections (did you know 52% of people get fungal infections after visiting nail salons?) If you decide to trim your toenails at home, make sure you invest in quality toenail clippers and avoid cutting them too short.
Proper foot hygiene
Wash your feet daily with soap and water, ensuring they dry thoroughly, especially between the toes. Also, wear flip flops in public spaces to avoid contracting fungal infections.
Comfortable footwear
Choose shoes that fit well and provide adequate support. Avoid narrow or tight shoes that can put pressure the toenails and contribute to thickening.
Moisturize regularly
Apply moisturizer to your feet to keep the skin and nails hydrated. This can prevent cracking and thickening of the toenails, especially in dry climates.
Foot protection
Wear protective footwear in risky environments like communal areas or outdoors. This can help prevent injury and reduce the risk of fungal infections.
Manage underlying conditions
If you have underlying health issues like diabetes, it's important to remember that they can be effectively managed. By working closely with your healthcare provider, you can improve foot circulation and reduce the risk of complications like toenail thickening.
June 3, 2024
Do orthopedic shoes have their place in fashion? The answer is yes! While there is no doubt orthopedic shoes are designed to treat foot conditions, it doesn’t exclude them from contemporary 2024 shoe trends. Let’s review the top choices for stylish orthopedic shoes this year!
Stylish Orthopedic Footwear 2024
Orthopedic shoes usually have specific features, such as:
Built-in arch support for plantar fasciitis, etc.
Extra cushioning / shock absorption (protects your joints from the impact of the ground!)
A wide toe box for foot deformities like bunions, hammertoes, etc.
Removable insoles to give you the option of using orthotics.
A firm heel counter for proper stability or motion control.
Adjustable straps to accommodate edema (swelling) and for a snug, breathable fit.
That’s a lot to look for! And it’s a common misconception that these features look unappealing. The truth is, you can't often see these features at first glance; orthopedic shoes do not have to look clunky.
If you’re not sure where to look for comfortable and fashionable shoes, keep reading for some examples that offer the best of both worlds. The cherry on top? All of them are available at Feet First Clinic!
Anodyne No. 27
Anodyne No. 27
Anodyne shoes are designed to help treat diabetes-related foot problems and other musculoskeletal issues and deformities. The No. 27 is a simplistic white walking shoe that pairs perfectly with casual attire. Features include a rigid heel counter to help with instability, a protective toe box, a supportive sole, and more. It's a comforting staple that keeps modern fashion trends in mind!
APEX Logan Chelsea Boot
The Logan Chelsea Boot from APEX offers a good amount of depth, and a removable EVA insole to boot (no pun intended!). The side zipper and lack of laces makes it easier for people with mobility challenges to get their feet in and out. This boot is also perfect for every season, from spring all the way to winter!
APEX LOGAN CHELSEA BOOT
Aetrex Men's Milos And Women's Jess
Aetrex is a cutting edge company offering trendy orthopedic shoes. The men's Milos are an orthopaedic slide sandal that combines the comforting and supportive features you would typically find with a custom orthotic, with the breathability and stylish flair of a summer sandal. They're super durable and have great arch support and cushioning thanks to UltraSky™ EVA technology.
Like the Milos, the Jess from Aetrex is another sandal offering the same top-of-the-line arch support and cushioning. The microfibre top cover adds a layer of softness and fights against cuts, scrapes and blisters. One minor difference is the easily adjustable ankle strap for extra ankle support.
NAOT Amadora
Looking for a fashion-forward sandal with a slight platform and fun design? The NAOT Amadora is a great finishing touch for your everyday summer dresses, skirts, and more! The hook and loop strap with full upper coverage is great for those who prefer a more secure feel to their sandals. The removable, anatomic cork and latex footbed conforms to the natural shape of your foot as it moves, offering maximum comfort! The best part: the footbed is removeable so you can wear them with your custom orthotics!
Naot Amadora
May 20, 2024
As the temperatures rise and the sun shines brighter, it's time to ditch the closed-toe shoes and slide into something more comfortable and breathable. Yes, it's sandal season! But with so many options available, how do you choose the best sandals for your summer adventures? We've got you covered.
In this guide, we'll explore the essential features to look for in summer sandals and introduce you to some top picks that seamlessly blend style with comfort.
Cork footbed
One key feature to consider when selecting summer sandals is the footbed material. Cork footbeds are famous for their ability to mould to the shape of your foot over time, providing personalized support and cushioning.
Additionally, cork is lightweight and absorbs shock, making it an excellent option for all-day wear. Whether strolling along the boardwalk or exploring a new city, sandals with cork footbeds ensure your feet stay comfortable and supported.
Arch support
Arch support is essential, especially if you plan on wearing your sandals for extended periods. It distributes weight across your feet, reducing strain and preventing discomfort. A lack of arch and forefoot support can lead to foot problems like plantar fasciitis or metatarsalgia.
Look for sandals with arch support or removable insoles. You can customize the level of support to your liking. Your feet will thank you after a long day of sightseeing or outdoor activities.
Backstraps for support
While slip-on sandals are convenient, they may provide a different level of support and stability than those with backstraps.
Backstraps help secure the sandals to your feet, preventing them from slipping and sliding with each step. Added stability is particularly beneficial if you plan to engage in more active pursuits or tend to pronate or supinate. Backstraps come in various styles, from adjustable buckles to elasticized bands, allowing you to find the perfect fit for your feet.
Our top picks
Now that we've covered the essential features to look for in summer sandals let's introduce you to some top picks that effortlessly combine style with comfort.
NAOT Cornet and NAOT Castelo
Best for cork footbeds
With their contoured cork footbeds and adjustable backstraps, NAOT sandals offer exceptional comfort and support. The NAOT Cornet and NAOT Castelo styles feature chic designs that transition seamlessly from day to night.
Mephisto Hester and Mephisto Hetty
Best for cork footbeds
Mephisto sandals are renowned for their superior craftsmanship and comfort technology. The Mephisto Hester and Mephisto Hetty models boast cushioned footbeds with arch support and durable backstraps for added stability.
Aetrex Jess
Best for arch support
The Aetrex Jess sandals feature a built-in Lynco orthotic footbed for maximum support and alignment. The adjustable backstrap ensures a secure fit, making them ideal for all-day wear.
NAOT Enid and NAOT Amadora
Best for backstrap support
NAOT offers a range of stylish sandals with cork footbeds and backstrap designs. The NAOT Enid and NAOT Amadora are built with quality and comfort in mind. The three variations three are perfect for summer adventures.
Mephisto Norine
Best for backstrap support
The Mephisto Norrine sandals combine elegance with functionality. Featuring Soft-Air technology and adjustable straps, they provide unparalleled comfort and support for any occasion.