June 10, 2024
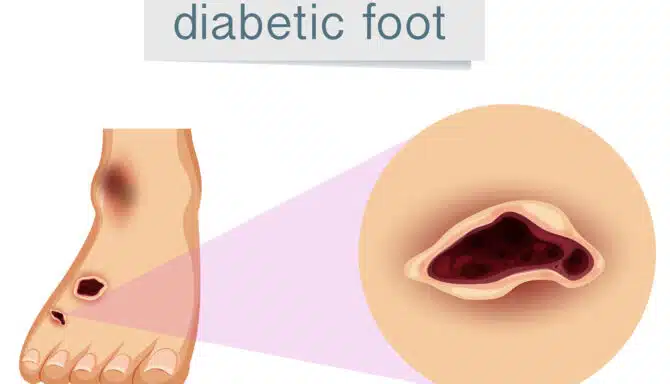
Not fully understanding of diabetes complications and the importance of preventative diabetic foot care can be detrimental. Diabetic ulcers (sometimes called diabetic foot) often occur after the onset of diabetic neuropathy, which severely restricts sensation in the feet. Around 40-50% of diabetes patients develop neuropathy; people with type 1 diabetes may develop it years after their diagnosis, while those with type 2 can sometimes already have neuropathy in the pre-diabetes stage.
Today, we’ll explore how minor cuts and scrapes, combined with neuropathy, can lead to ulcers and progressively severe issues. But with solid diabetes awareness and preventative measures, serious complications can be easily avoided!
How Cuts and Scrapes Turn Into Diabetic Ulcers
Here are the five stages between a tiny wound and a full blown diabetic ulcer:
Stage 1: Initial Injury
A minor injury such as a cut or scrape occurs on the skin — anything from a small burn to stepping on a piece of glass. Foot conditions that open the skin’s barrier can also cause tiny wounds, like blisters, cracked heels, calluses and ingrown toenails. For individuals without diabetes, these usually heal without complications.
Stage 2: Diabetes Impairs Circulation and Wound Healing
Diabetes and diabetic neuropathy halts the wound healing process, especially if diabetes is uncontrolled. First, high blood sugar levels harm blood vessels and restrict the oxygen-rich blood flow our injuries need for repair. Neuropathy also causes a loss of sensation, meaning you may not even be aware of the cut or scrape.
Stage 3: Infection
The wound may become red, swollen, and warm, indicating infection. Pus or an unusual discharge might be present.
Stage 4: Chronic Wound
The cut or scrape evolves into a chronic wound, characterized by persistent inflammation and failure to heal after several weeks.
Stage 5: Diabetic Ulcer
An ulcer forms as an open red or pink sore that looks “punched out.” It may penetrate deeper layers of skin, extending to muscle or bone in severe cases. Tissue death (necrosis) can also occur, leading to blackened areas around the ulcer. Ulcers can lead to extensive tissue death (gangrene) and bone infections when ignored.
What You Can Do to Prevent Diabetic Ulcers
Ulcers sound scary, but the good news is that being vigilant about your foot health can help keep your feet ulcer-free. Examine your feet at home every day, keep them clean, and wear protective orthopedic slippers while inside to protect your skin. Lastly, you should regularly visit your chiropodist for inspections and diabetic foot care if you have diabetes; ask them how frequently you should be coming in!
June 3, 2024
Do orthopedic shoes have their place in fashion? The answer is yes! While there is no doubt orthopedic shoes are designed to treat foot conditions, it doesn’t exclude them from contemporary 2024 shoe trends. Let’s review the top choices for stylish orthopedic shoes this year!
Stylish Orthopedic Footwear 2024
Orthopedic shoes usually have specific features, such as:
Built-in arch support for plantar fasciitis, etc.
Extra cushioning / shock absorption (protects your joints from the impact of the ground!)
A wide toe box for foot deformities like bunions, hammertoes, etc.
Removable insoles to give you the option of using orthotics.
A firm heel counter for proper stability or motion control.
Adjustable straps to accommodate edema (swelling) and for a snug, breathable fit.
That’s a lot to look for! And it’s a common misconception that these features look unappealing. The truth is, you can't often see these features at first glance; orthopedic shoes do not have to look clunky.
If you’re not sure where to look for comfortable and fashionable shoes, keep reading for some examples that offer the best of both worlds. The cherry on top? All of them are available at Feet First Clinic!
Anodyne No. 27
Anodyne No. 27
Anodyne shoes are designed to help treat diabetes-related foot problems and other musculoskeletal issues and deformities. The No. 27 is a simplistic white walking shoe that pairs perfectly with casual attire. Features include a rigid heel counter to help with instability, a protective toe box, a supportive sole, and more. It's a comforting staple that keeps modern fashion trends in mind!
APEX Logan Chelsea Boot
The Logan Chelsea Boot from APEX offers a good amount of depth, and a removable EVA insole to boot (no pun intended!). The side zipper and lack of laces makes it easier for people with mobility challenges to get their feet in and out. This boot is also perfect for every season, from spring all the way to winter!
APEX LOGAN CHELSEA BOOT
Aetrex Men's Milos And Women's Jess
Aetrex is a cutting edge company offering trendy orthopedic shoes. The men's Milos are an orthopaedic slide sandal that combines the comforting and supportive features you would typically find with a custom orthotic, with the breathability and stylish flair of a summer sandal. They're super durable and have great arch support and cushioning thanks to UltraSky™ EVA technology.
Like the Milos, the Jess from Aetrex is another sandal offering the same top-of-the-line arch support and cushioning. The microfibre top cover adds a layer of softness and fights against cuts, scrapes and blisters. One minor difference is the easily adjustable ankle strap for extra ankle support.
NAOT Amadora
Looking for a fashion-forward sandal with a slight platform and fun design? The NAOT Amadora is a great finishing touch for your everyday summer dresses, skirts, and more! The hook and loop strap with full upper coverage is great for those who prefer a more secure feel to their sandals. The removable, anatomic cork and latex footbed conforms to the natural shape of your foot as it moves, offering maximum comfort! The best part: the footbed is removeable so you can wear them with your custom orthotics!
Naot Amadora
April 25, 2024
Foot reflexology benefits are becoming a hot topic. Studies show that published scientific articles on the subject are increasing, piquing public interest. But is there a reason to subscribe to holistic foot care? Can foot reflexology techniques truly benefit our health or treat common foot conditions? And if so, how does reflexology for health work? Let’s answer all of these questions today!
How Does Foot Reflexology Work?
Foot reflexology is a holistic practice. It involves applying pressure to specific points on the feet, known as reflex points, which correspond to various organs, glands, and parts of the body via an energetic connection. By stimulating these points, the goal is to help with a wide variety of ailments and health concerns.
For example, the toes may correspond with the head and brain, the ball of the foot with the diaphragm and arms, and the area of the foot between the ball and heel corresponds with the small intestine.
Check out this detailed chart from Healthline for more.
How Reflexology May Help With General Health Problems
Reflexology may be a good option for you if you experience any of the following:
Premenstrual symptoms: A significant study demonstrated that foot reflexology could effectively reduce cramping and hormonal side effects. Participants were observed after 8 foot reflexology sessions.
Blood pressure: Reflexology can sometimes reduce blood pressure in hypertensive patients. Don’t forget, your feet and your heart are connected in other ways too!
Mental illness: Holistic foot care may reduce anxiety and depression symptoms in adults.
Chemotherapy side effects: Foot reflexology may help reduce shortness of breath in cancer patients receiving chemotherapy.
Can Foot Reflexology Treat Foot Conditions?
Be sure to talk to your chiropodist if you are interested in trying new foot care treatments; this applies to reflexology or any type of unfamiliar service. It’s worth researching holistic foot care if you have any of these conditions:
Plantar fasciitis: Reflexology techniques involving pressure points and trigger point release may reduce heel pain.
Heel spurs: See note on plantar fasciitis above.
Osteoarthritis: Holistic foot care may stimulate blood circulation, mildly relieving joint stiffness.
Diabetic neuropathy / Diabetes Mellutis: Studies indicate that foot reflexology may help increase skin sensation and reduce blood sugar levels.
April 11, 2024
You are what you eat! This statement could not be more true, as the foods we consume help our bodies function at their best. The connection between nutrition and foot health isn’t widely known or obvious, but a healthy diet can work wonders for bone and joint health in the lower extremities. Eating the right foods for strong feet may also help you avoid painful foot conditions when combined with other foot care practices. Keep reading to discover nutrition and foot health secrets!
How Good Nutrition Benefits Foot Health
Healthy eating can lead to stronger feet by helping prevent excess inflammation. Inflammation can be protective and healing, but on the flip side, too much can lead to the following:
Tissue damage
Joint degradation (arthritis)
Injuries and mobility issues
Reduced bone density
Moreover, a healthy diet supports proper blood circulation, which is essential for delivering oxygen and nutrients to the feet. Poor blood circulation can lead to cramping in the lower extremities, fatigue, varicose veins, and even ulcers, which are very dangerous for diabetics.
Lastly, when we fuel our bodies with whole foods and don’t overeat (it’s okay to indulge on occasion!), we can maintain a healthy weight. Living your life at a healthy weight poses many benefits for your feet, including:
Enhanced mobility and flexibility
Decreased strain on the foot (your feet are carrying less weight, which is extra important when you have flat feet)
Improved circulation to the feet
Less edema and water/salt retention
The Best Healthy Diet for your Feet
Now let’s get to the fun part — exploring all of the yummy and nutrient-rich foods you should eat for strong feet! Check below for a list of the top choices to help your feet feel great. Keep in mind you can eat many more foods than these; we just think these options stand out as foot health power foods!
Salmon: Rich in omega-3 fatty acids, which help reduce inflammation and promote joint health.
Leafy greens: High in vitamins and minerals like calcium, magnesium, and vitamin K, which are essential for bone health.
Berries: Packed with antioxidants that help reduce inflammation and improve circulation.
Nuts and seeds: Good sources of healthy fats, vitamins, and minerals that support overall foot health.
Greek yogurt: Contains calcium and probiotics, beneficial for bone density.
Turmeric: Contains curcumin, a compound with anti-inflammatory properties that can alleviate foot pain and swelling.
Avocados: Provides healthy fats and potassium, essential for maintaining proper muscle function and reducing cramping.
Beans and legumes: High in fiber, protein, and various nutrients that support overall health and can help prevent foot-related complications like diabetes.
To learn more about great foods for foot health, read here.
In terms of what to avoid or eat in moderation, foods that cause inflammation are the main culprits. These include:
Red and processed meats
Baked goods and pasta made with refined carbohydrates
Deep fried foods
High-sugar foods like candy and soda
Foods with trans fat (certain types of butter, chips, etc)
March 21, 2024
Foot hygiene and solid foot care tips are your secret weapons for happy and healthy feet! Everyone should practice a clean and healthy foot routine, but those with foot conditions such as diabetes or chronic fungal infections should be extra vigilant. Today we’ll talk about the best foot cleaning practices and how to implement them into your daily foot care routine.
Foot Health Essentials: How to Keep Your Feet Clean and Protected
Foot hygiene is pretty straightforward stuff! But you may make some minor missteps along the way. Take a look below at the best ways to wash, dry and moisturize your feet.
Washing Your Feet
Wash your feet daily with natural, gentle soaps in warm water. Hot water can negatively impact your blood circulation by increasing the size of the blood vessels, so be careful with temperatures.
Moisturizing Your Feet
Use lotion on the bottom and top of your feet. This can help you prevent calluses, corns, cracked heels, and more. Natural, fragrance-free and medicinal lotions are your best bet (try Gehwol at Feet First Clinic!). If you have diabetes, be extra careful to avoid putting lotion in between your toes; it could cause an infection depending on the lotion. Fungal infections also favour wet toes and tend to appear there.
Keeping Your Feet Dry
Thoroughly dry your feet after washing them. If you get lazy and keep them damp, you are again more likely to attract contagious fungal infections (they love moist environments!).
Invest in products that help manage foot dampness and repel excess moisture. These include moisture-wicking socks (also remember to change your sock frequently!), waterproof shoes and boots, running shoes with perforated holes in the uppers, and various foot deodorant products (creams, powders, sprays). These products are also great for preventing foot odour.
Toenail Care and Foot Hygiene
Keeping your nails in top shape is an important element of foot hygiene. Follow these nail care tips to protect your nails and keep them clean and strong.
Cut your nails straight across with high-quality nail clippers. Don’t try to shape them during this stage!
Avoid cutting your nails too close to the skin; this will cause ingrown toenails.
Gently use a nail file for subtle shaping.
Don’t try to cut your own cuticles if you’re prone to infections. They protect the nails and getting rid of them improperly may welcome fungi.
Schedule a medical pedicure for professional care and a cleaning of hard-to-reach areas.
March 7, 2024
Foot health directly correlates with our overall wellness. Seniors, in particular, can learn a lot about their general health when they start to understand the biomechanics of healthy feet. How feet look, how they feel, and how they function can be a sign of a serious health issue. This is also true in reverse — neglecting foot health can lead to conditions and other problems. Let’s take a look at how our feet act as a mirror to our holistic health. Here are the two main topics we'll break down today:
How our feet can signify poor health
How neglecting foot health affects overall wellness
How Our Feet Can Signify Poor Health
Your feet will often try to warn you that you need to visit your family doctor or foot specialist. Some of these warning signs include:
Cold feet
Feet that are cold to the touch and don’t seem to warm up can be a sign of a blood circulation or heart issue. Icy cold feet can also be a sign of peripheral artery disease, which is the narrowing or blockage of blood vessels in the lower extremities, or a thyroid condition.
Sores and wounds that don’t heal
Diabetes is arguably the medical condition most notorious for damaging our feet. Elevated blood sugar levels can make our feet more susceptible to wounds. Even the tiniest blister, cut, or callus that doesn’t bother the average person can become a major concern. Wounds that do not heal can become infected and lead to devastating problems like gangrene and amputation.
Numbness and tingling
Bizarre foot sensations are also often a tell-tale sign of diabetes. They warn us that diabetes has progressed to the point of neuropathy (when the disease causes nerve damage).
Foot swelling (edema)
Injuries, medications, heart and kidney problems, and more can all cause fluid to accumulate in the tissues. Edema can also be a sign that you need to eat less salty foods.
Foot pain
From plantar fasciitis to Morton’s neuroma, painful feet can be a sign of many conditions, and it’s tough to really narrow down the cause. Sometimes it may be from simply ignoring foot care for years (wearing unsupportive shoes, not using inserts or orthotics, etc), but sometimes it may be a sign of age-related joint deterioration, like osteoarthritis, or weight gain.
Strange colouring
Toes that turn red, white or blue may be a sign of Raynaud’s disease (this can also make your feet very cold). This condition often causes blood vessel “spasms” due to their narrowing, and may be connected to stress and cold weather.
How Poor Foot Health Affects Overall Wellness
Taking care of your feet plays an imperative role in an overall healthy lifestyle. Everyone should practice foot care, but foot health tips for seniors are extra important as we age.
Outside of foot pain and the common foot conditions we all know about, here are some other ways poor foot health can affect you:
Back, knee and hip pain
Foot issues may contribute to pain and discomfort in the back, knees, and hips due to altered gait and poor posture. This happens when you adopt unusual walking patterns to make up for the fact that your normal stride is painful. Remember, the musculoskeletal system is all connected!
Heightened injury risk
Weaker feet = more likely to fall and do some serious damage. Ignoring things like strengthening exercises and wearing proper footwear can lead to vulnerable feet.
Infections
Don’t ignore skin and toenail issues and assume they will magically go away! We already touched on how important this is for diabetes patients, but brushing off problems like fungal conditions can lead to painful infections that may even harm your immune system. This is true for everybody.