Diabetes is a serious illness that affects people from all over the world. Type 1 or type 2 diabetes can lead to several complications, like heart disease, kidney problems, vision issues, oral health deterioration, and more. But one of the most common problems diabetes patients face is diabetic foot pain and other foot problems that can transform into serious complications when left unchecked.
Today’s blog will discuss the following:
- The causes of diabetic foot pain
- Diabetes-related foot complications
- Diabetic foot pain treatment at a foot clinic
- Self-care tips and at-home diabetic foot care

What Causes Diabetic Foot Pain?
The main culprit behind type 1 and type 2 diabetes-related foot pain is diabetic neuropathy. Diabetes patients struggle with four types of neuropathy, all of which cause nerve damage:
- Peripheral Neuropathy: This is the most relevant categorization of neuropathy when discussing foot pain causes. It affects the lower extremities (feet and legs), arms and hands. It occurs when high blood sugar and triglyceride levels damage the nerves and tiny blood vessels in the circulatory system, causing poor blood flow. Symptoms include shooting foot pain, “pins and needles,” numbness, weakness and burning sensations.
- Autonomic Neuropathy: This is similar to peripheral, except the nerve damage affects the body’s organs rather than the limbs.
- Proximal Neuropathy: A rare type of nerve damage that causes severe hip, buttock, or thigh pain.
- Focal Neuropathies: Rare singular/local (hence “focal”) nerve damage, typically in the hand, head, torso, or leg.
Diabetes-Related Foot Complications
Whether it’s numbness or pain, it is extremely important to pay attention to the warning signs your feet give when you have diabetes.
Moreover, your feet often fail to signal problems to your brain due to neuropathy. This means you also need to consistently inspect your feet and visit a foot specialist for an extra set of eyes and expertise (more on that later!)
If you don’t, debilitating complications with varying degrees of pain and discomfort may creep up. These include:
- Skin changes like dry skin and cracked heels. This occurs due to nerve damage preventing your body’s natural oil and moisture production.
- If you cannot feel cold, heat and other sensations on your feet, you may be unaware of a foot injury. This can lead to a worsening injury or infection if the skin is broken and you haven’t noticed.
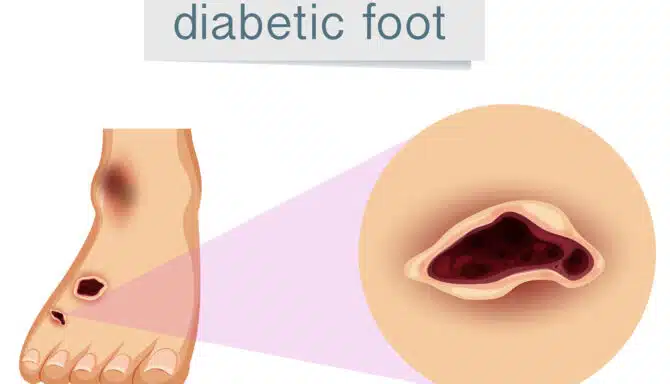
- Calluses are common in people with diabetes, and the more they thicken, the more likely they are to become an ulcer (open sores or lesions that will not heal).
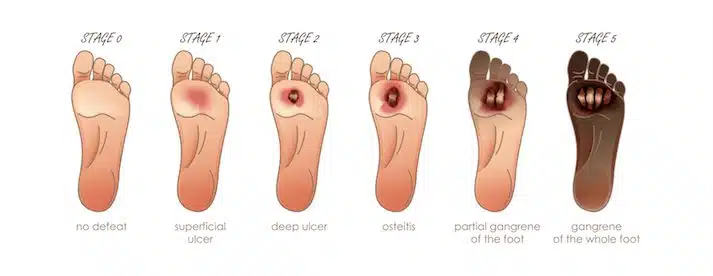
- Peripheral artery disease (plaque buildup in the arteries) can arise in diabetic patients. Like neuropathy, it reduces blood flow, so you don’t notice ulcers, infections and injuries. Aggressive infections and ulcers without treatment can lead to gangrene or amputations.
- Edema (swelling): This is caused by nerve damage and the subsequent fluid buildup in the body’s lower extremities. Swelling can cause pain and mobility problems.
Diabetic Foot Pain Treatment at a Foot Clinic
Since diabetes impacts our feet, patients should find a chiropodist and schedule regular appointments. The general recommendation is no less than once yearly but more frequently if nerve damage is present.
Not only can foot specialists help with pain management, but consistent foot inspections are critical for spotting the beginning stages of a complication.
Some of the main ways chiropodists help with diabetic foot pain include:
- Skin health assessments and maintenance
- Foot assessments
- Custom orthotics
- Footwear recommendations
Skin Health Assessments and Maintenance
This is one of the most important jobs a chiropodist will do. They can notice signs of ulcer development, infections and other skin abnormalities. Chiropodists also perform regular diabetic foot care on diabetes patients, so they don’t develop ingrown toenails or fungal infections.
Foot Assessments
Your chiropodist will check your vascular (circulation) health via regular inspections. They will also check your foot temperature, look for swelling, and check the colour of your feet. They can also ask what type of foot sensations you’re feeling, like tingling, shooting pain or burning and proceed from there. This is included with Feet First Clinic’s diabetic foot care services.
Custom Orthotics
Orthotics make walking much easier, as they distribute body weight evenly across the foot while reducing pressure and friction and relieving the foot’s pressure points. They also help regulate your motion and correct any abnormal gait patterns you develop while struggling with foot pain. Chiropodists can provide orthotics via a thorough a biomechanical assessment.
Footwear Recommendations
Footwear modifications can help reduce diabetic foot pain, and the special shapes and designs of orthpaedic footwear can accommodate neuropathy symptoms more successfully than standard footwear. Diabetic patients often need deep shoes to support orthotics and to manage the discomfort and pain they experience when dealing with swelling. Diabetes patients also need footwear with little to no seams in order to reduce pressure points and friction against the foot. Companies such as APEX and Anodyne make shoes especially for diabetes patients.
Self-Care Tips and At-Home Diabetic Foot Care
- Orthopedic slippers can help manage foot pain and allow you to move around your home more freely.
- Soak your feet in a warm foot bath to ease stress and soothe aches and pains.
- Try your best to regulate blood sugar levels to help fight nerve damage.
- Inspect your feet and keep them clean. Note: do not try to get rid of calluses and other skin abnormalities on your own. Schedule an appointment with your chiropodist if you notice callus buildup or skin problems.
- Keep on top of diabetes routines not directly related to your feet. This includes proper medication management and regularly checking your blood pressure at the local pharmacy and doctor’s office.
- Light exercises and stretches can be beneficial for diabetic foot pain. For example, rolling your feet on a ball (or water bottle) or scrunching your toes to pick up a towel can strengthen your feet. And those are just two examples! Most foot stretches are easy to perform and relieve pain in different ways. Low-impact activities like swimming and walking can also be beneficial.