April 18, 2024
Innovation has always been important in the healthcare world, with chiropody and innovative foot treatments being no exception! These days, with advanced foot care, you can enjoy pain management and comfort without resorting to a time-consuming ordeal like surgery. Let’s explore the services you can participate in thanks to innovation and great ideas!
Innovative Treatments for Common Foot Problems in 2024
Confusing and lengthy procedures can cause you to neglect the foot condition you may be struggling with, so modern treatments should save you time and put you at ease! Here are some of the best innovative treatments available today:
Shockwave therapy
Custom orthotics
Video gait analysis
Onyfix
Splinting and taping
Shockwave Therapy
Healthcare professionals have been using shockwave therapy to address musculoskeletal conditions since the 1980s. While the term “shockwave” can be off-putting, it’s a totally non-invasive procedure and most patients report very mild discomfort and no pain.
Shockwave therapy is quickly shaping up to be one of the best Achille’s tendonitis, Morton’s neuroma, and plantar fasciitis solutions. It works by targeting injured tissues, boosting blood circulation and stimulating a natural healing response in our bodies.
To learn more about shockwave therapy, click here.
https://youtube.com/shorts/nt1SgT9xrUM?si=8Qb-k95qUnNje57U
Custom Orthotics
Orthotics date back to ancient civilization when humans started to realize their feet needed more support! As the centuries passed, they have become one of the most innovative treatments because now chiropodists and manufacturers can mold them to fit your specific needs. Custom orthotics treat a wide range of conditions and help correct your gait.
To learn more, click here.
https://youtube.com/shorts/IBXAXoUouFY?si=1EmiGsgLUrMAq70a
Video Gait Analysis
A video gait analysis uses technology and visuals to determine what type of unique gait (walking pattern) you have. Think of it as a much more advanced version of walking on a treadmill! It gives your chiropodist the insight they need to help you correct it and avoid pain as much as possible.
To learn more, click here.
https://youtube.com/shorts/Rhuga6vLdc0?si=nZf7o5Dx-oe2tUc_
OnyFix
Imagine if you could alter your nail growth pattern without using invasive tools? Primarily used as an ingrown toenail treatment, OnyFix uses composite material to ensure your nails grow evenly and correctly! It’s one of the newest chiropody treatments and only became popular in North America within the past decade or so.
To learn more, click here.
https://youtube.com/shorts/ZsFQqCkVf40?si=u-Z_6MQ90GjgDpV_
Splinting, Taping and Correction
Tapes, splints and other devices can help people manage foot deformities without surgeries. For example, patients often experience bunion relief with bunion correctors, which are both affordable and comfortable and put your toes in an optimal position. Splinting and taping can also do the same for various conditions!
To learn more, click here.
September 14, 2023
Bunions - or for those who have them, the painful, bony nuisances that form at the big toe joint - are a common foot condition for older people, especially women. While surgical intervention can sometimes help those with debilitating bunions, lifestyle changes and effective management strategies can help you avoid a bunionectomy in many cases.
Moreover, surgeries are usually only necessary if your bunions cause regular functional and mobility problems and chronic pain, which is often not the case.
Let’s look at the causes and symptoms of bunions and explore how you can manage them without invasive measures.
Image Credit: Fabrikasimf from Freepik
Symptoms of Bunions
Bunions protrude from the side of your big toe, forming an “L” shape angle. Additional symptoms of bunions include:
More corns and calluses than you would normally have due to the big toe rubbing against the second toe
Mild redness, pain, and swelling
Limited movement in the big toe
Severe bunions can cause overlapping toes, pain that doesn’t subside, and toe angulation of more than 40 degrees.
Photo credit: istock
Causes of Bunions
The main culprit? The wrong shoes!
Wearing high heels may make you feel good about yourself aesthetically, but they can damage your physical health over time and are one of the main causes of bunions in women. Narrow, tight, and pointed shoes (often the design of stilettos and other types of heels) squeeze and push your toes together and forward unnaturally, increasing pressure on the big toe and leading to bunion formation.
Having another condition that targets the joints, like osteoarthritis or Rheumatoid arthritis, or one that causes an abnormal gait, like flat feet, can also hint at bunions in your future. Activities where your toes are more vulnerable than the rest of your feet, like dancing, may also be a risk factor.
Image by rawpixel.com from FreePik
Bunions: Management Strategies
You can tackle a mild bunion problem from home and with regular visits to the chiropodist. Here are some of the best ways you can prevent bunions from ruining your day or getting worse:
Change your footwear: Ditch the high heels for comfortable alternatives and shoes with extra room in the toe box. If you’re not sure where to start, attend a shoe fitting.
Try bunion splints or aligners. They can hold the affected joint in place.
Therapeutic taping can help hold the joint in place and temporarily relieve pain.
Shoe stretching may help secure more room in the toe box and take pressure off the bunion.
Try these 5 simple exercises for bunions. They are relatively easy, low-impact, and don’t require exercise equipment.
Get custom orthotics. Orthotics might reduce excess pressure on the big toe joint and correct any biomechanical issues that are contributing to your bunions (plus they're also super comfortable!).
Ask about shockwave therapy. This innovative, non-invasive, and quick procedure is an effective management strategy for bone and joint conditions. It can help relieve pain caused by muscle tightness around the bunion.
It's important to remember that bunions don't disappear like other conditions sometimes do. But successfully practicing these treatment methods can help you avoid surgery.
If you suspect your bunions are too severe for these strategies, speak to your family doctor.
Bunion products available at Feet First Clinic
July 24, 2023
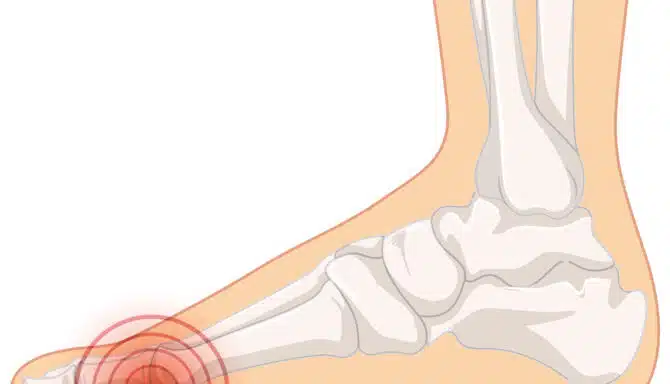
Heel spurs are bony growths on the heel bone that look like small bumps on the heel. Although they can’t be removed entirely without surgery, there are several non-surgical treatment options that can provide heel spur relief and maximize your quality of life.
Heel spurs often cause pain and discomfort, especially during weight-bearing activities. The most common form is called a calcaneal spur, which is a bony projection that forms around the calcaneal bone, the strongest, most significant, and posterior-most bone in the feet.
Surgery is only sometimes the best option. Exhausting non-surgical treatment options should come before more intrusive options, especially considering heel spur pain can be managed in several ways. If conservative measures do not provide relief or the pain worsens, you should consult a healthcare professional or foot specialist who can evaluate the condition and recommend further treatment options.
This article outlines some non-surgical treatment options and lifestyle changes for heel spur relief.
Regular rest and icing
Resting the affected foot and applying ice packs for 15-20 minutes several times daily can help reduce inflammation and pain. Allowing adequate rest between activities or when your heel spur flares up provides time to reduce inflammation and swelling. Additionally, rest allows the surrounding muscles to rebound and recover so you don’t overstress certain parts of your foot.
Pain relief medication
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help alleviate pain and reduce inflammation associated with heel spurs. However, following the recommended dosage and consulting a healthcare professional is essential.
Physical therapy
Specific exercises and stretches can help elongate and strengthen the muscles and tendons in the foot, providing relief from heel spur pain. A chiropodist can recommend the proper exercises to incorporate into your routine to help strengthen and stretch the calf muscle, which is often the culprit for heel pain. Regularly performing stretching exercises for the calf muscles and plantar fascia can help relieve tension and reduce pain associated with heel spurs. These sorts of exercises and stretches shouldn’t just be done when you’re in pain. Incorporate them into your daily routine as part of your lifestyle.
A chiropodist may also recommend treatments such as shockwave therapy, a non-invasive treatment method that uses soundwave pulses. While the name may cause you to assume electrical impulses are at work, they’re actually mild-frequency soundwaves. These soundwaves penetrate through the skin at the site of an injury, which triggers your body to amp up its healing abilities. Very little (if any) pain is involved in the process.
Custom orthotics or inserts
Custom or over-the-counter orthotic shoe inserts can help support the arch and cushion the heel, reducing pressure on the heel spur and providing pain relief. These inserts can be used in both athletic and everyday shoes. You can supplement your shoes with heel cushions or pads for extra heel relief.
Supportive footwear
Wearing shoes that provide proper arch support, cushioning, and shock absorption can help alleviate heel spur pain. Look for shoes with a padded heel and good arch support. For instance, ASICS provides a variety of lines of shoes for various foot types.
Night splints
Wearing a night splint while sleeping can help stretch the plantar fascia and calf muscles, reducing morning heel pain associated with heel spurs. Heel spur pain is typically at its most intense in the morning, and wearing a night splint helps stretch out your calf, reducing tension on your heel during the first few steps of the day.
Weight management and diet
Maintaining a healthy weight, specifically aiming to reduce sudden and significant fluctuations in weight, can help alleviate stress on the feet and reduce heel spur pain. Sudden weight changes or changes to diet can put added stress on your feet and legs while your body adjusts. Following a healthy diet while also exercising can help improve the feeling of your feet and body overall.
March 27, 2023
Do you experience heel pain when you walk or stand? Is the pain exceptionally sharp in the mornings or evenings? You might have a foot injury called plantar fasciitis.
Plantar fasciitis is a common condition that causes pain and inflammation in the heel and bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that runs from the heel to the toes, becomes strained or injured. This can cause tiny tears in the fascia, leading to pain, swelling, and stiffness.
In this blog post, we explore what is plantar fasciitis, its common symptoms, and treatment options.
What is plantar fasciitis?
Plantar fasciitis is pain or soreness in the heel and sole. It occurs when the band of tissue between your heel and toes on the underside of the foot - called the plantar fascia - becomes inflamed or irritated.
The plantar fascia absorbs shock and supports the arch of the foot. Small tears can occur in the tissue when it is repeatedly strained, leading to inflammation and pain. This condition is common in athletes, runners, and people who stand for long periods.
Most common symptoms of plantar fasciitis
Plantar fasciitis symptoms includes:
Sharp or stabbing pain in the heel or arch of the foot, especially in the morning or after periods of rest.
Pain that worsens with weight-bearing activity or standing for long periods.
Stiffness or aching in the bottom of the foot.
Swelling or redness in the heel or arch.
The most common symptom of plantar fasciitis is a pain in the heel or arch of the foot. You may experience pain in the surrounding areas due to plantar fasciitis, but discomfort is typically in the underside of the midfoot.
Pain can be more intense during certain times of the day. You may experience plantar pain, even a sharp stabbing sensation, in the morning and evening.
Next, let's tackle effective treatment methods for plantar fasciitis to help you recover from this foot condition as soon as possible.
Plantar fasciitis treatment methods
Plantar fasciitis treatment depends on the severity and longevity of the pain. Try the following treatment methods to see what works best for you.
RICE: Rest, Icing, Compression, and Elevation
The "RICE" method is a commonly recommended treatment for minor injuries, including sprains, strains, and bruises. RICE stands for:
Rest: Reduce and avoid activities that exacerbate the pain, and rest the foot as much as possible. Resting may include taking a few days off exercise or wearing more supportive shoes around the house to strengthen your feet.
Ice: Use cold therapy by applying an ice pack or dipping your feet in an ice bath or tub for 15-20 minutes to reduce inflammation and pain.
Compression: Compression sleeves can help reduce swelling and improve blood flow to the feet and legs. You can also choose to wear a splint at night to stretch the plantar fascia and Achilles tendon while sleeping.
Elevation: Lifting your feet above your heart by elevating your legs and feet can reduce swelling.
The RICE method works best in the first 48 to 72 hours after injury or aggravation, but can be effective throughout the treatment stage. Afterward, you may gradually move the affected area and do gentle exercises to help you recover.
Shockwave therapy
Shockwave therapy is a non-invasive medical treatment that leverages sound waves to kickstart healing. A handheld device delivers the waves on the underside of the foot.
The high-energy sound waves stimulate the growth of blood vessels and encourage better blood flow to the affected area. Greater blood flow can help reduce pain and inflammation and promote tissue regeneration.
Shockwave therapy requires a series of sessions. Each session last 10-15 minutes, and the number of sessions varies based on the severity of the injury.
Did you know Feet First Clinic offers shockwave therapy for plantar fasciitis? Book an appointment online or call us at (416) 769-3338.
Stretching exercises
Stretching exercises can help relieve the symptoms of plantar fasciitis. Specifically, stretching the plantar fascia and the Achilles tendon can effectively treat heel and arch pain.
Here are some stretching exercises that may help with plantar fasciitis:
Calf stretch. Stand facing a wall with your hands on the wall at shoulder height. Step back with one foot and keep it straight, with the heel on the floor. Lean forward with the other foot, keeping both heels on the floor until you feel a stretch in your calf.
Plantar fascia stretch. Sit in a chair with one foot on your opposite knee. Grab the base of your toes with one hand and your heel with the other. Gently pull your toes back toward your shin until you feel a stretch in the arch of your foot.
Towel stretch. Sit on the floor with your legs straight out in front of you. Place a towel around the ball of your foot and hold both ends of the towel with your hands. Pull the towel toward your body until you feel a stretch in your calf and the bottom of your foot.
Generally, we recommend holding stretches for 20-30 seconds and switching sides. You should feel a light stretch and shouldn't strain the movement, or you risk overextending your muscles.
Orthotics
Custom orthotics are shoe inserts that fit your feet and address biomechanical issues that may contribute to plantar fasciitis. Custom orthotics can help curb plantar fasciitis by doing the following:
Reduce pressure on the plantar fascia by redistributing pressure away from the plantar fascia, which can help reduce pain and inflammation.
Correct foot mechanics, including flat feet or collapsed arches.
Provide cushioning and support.
Improve overall foot function by addressing underlying biomechanical issues and providing support and cushioning to the foot.
It's important to note that custom orthotics are not a one-size-fits-all solution and may not be appropriate for everyone with plantar fasciitis. Consult a chiropodist to determine if custom orthotics are right for you.
Taping
Taping isn't just for athletes. Elastic therapeutic taping techniques can limit unwanted movements that increase strain on the plantar fascia. Taping can act as a lock on your feet to reduce overextending any aggravated muscles in your feet. Research finds that "in the short-term, taping is beneficial in treating plantar fasciitis. The best evidence exists for low-dye taping and calcaneal taping."
The tape provides stability and structure to the muscle group. Our chiropodists at Feet First Clinic can tape your feet and toes to help treat plantar fasciitis.
Self-massage
Self-massage can be a helpful way to relieve some of the pain and discomfort associated with plantar fasciitis. Here are some techniques you can try at home:
Ball roll. Sit on a chair and place a tennis or massage ball under your foot. Roll your foot back and forth over the ball, applying pressure to the arch of your foot.
Thumb press. Sit on a chair and cross one leg over the other. Place your thumb on the arch of your foot and press firmly, moving your thumb in a circular motion. You can also use your other fingers to help support your foot and apply additional pressure.
Toe stretch. Sit on a chair and cross one leg over the other. Grab your toes with one hand and gently pull them back toward your shin until you feel a stretch in the arch of your foot. Hold for a few seconds and release.
Heel squeeze. Sit on a chair and place a small hand towel on the floor before you. Place your heel on the towel and squeeze your heel toward your toes, scrunching the towel.
A chiropodist can recommend additional exercises for you or demonstrate how to do these self-massage techniques to do them properly on your own.
March 20, 2023
Are you experiencing foot arch pain? You’re not alone.
The arches of our feet support our weight when we're upright, providing a critical function for the body. Your arch also influences how you move, making it essential to keep them healthy and supported. But, sometimes, pain can creep up.
We're here to help. This blog post outlines how foot arch pain develops and how to nip foot arch discomfort early to prevent long-term effects.
What is foot arch pain?
Foot arch pain can be a subtle or intense discomfort in the curved, raised area along the bottom of the foot (the arch). The arch is the midpoint of the foot between the ball and the heel of the foot. It comprises bones, ligaments, and tendons in the foot, which support the body's weight and help absorb shock during walking and other activities.
A person's arch is unique. The height and shape of the arch vary from person to person. Genetics, age, and the type of shoes a person wears all play a role in the arch's shape. Foot arch pain is a common source of discomfort and may occur for various reasons. You may experience pain in different parts of the arch: the medial arch (inside edge), the lateral arch (outer edge), and the transverse arch (middle).
Next, we get into the causes of foot arch pain.
What causes foot arch pain?
Foot arch pain can be acute or chronic, typically stemming from inflammation. Pain can also range from a dull soreness to an intense sensation. Below, we outline the various causes of foot arch pain.
Overuse or repetitive stress
Foot arch pain can be simply the result of doing too much in too short a period. Repeated stress or overuse of the feet can lead to inflammation and pain in the arches. Overuse is especially prevalent in sports, with running, jumping, or even standing for long periods (like at work or if you stand at your desk while working from home).
Flat feet
Flat feet occur when the arch comes in complete contact with the ground due to weakened tendons and ligaments that can no longer hold up the arch. While flat feet may not always cause problems, individuals with fallen arches may require treatment such as supportive shoes or custom orthotics to alleviate symptoms and prevent further damage.
Plantar fasciitis
Plantar fasciitis affects the bottom of the foot and causes heel pain. This foot condition occurs when the band of tissue between your heel and toes becomes irritated. Plantar fasciitis can happen for various reasons, such as overuse, repetitive strain, or injury to the foot.
People who are overweight, have flat feet or high arches, or engage in activities that stress the feet, such as running or standing for long periods, are more likely to develop plantar fasciitis. You may experience pain and stiffness in the heel or arch of the foot, especially in the morning or after walking, running, or standing.
Arthritis
Arthritis describes conditions that cause inflammation and damage to the joints. Various forms of arthritis can lead to arch pain. Types of arthritis that cause arch pain include osteoarthritis, rheumatoid arthritis, and psoriatic arthritis.
Injury
You may experience foot arch pain because of past trauma or injury. Conditions like sprains, strains, or falls can cause arch pain due to acute muscle damage, ligament, and tendon damage.
Now that you know the various causes of arch pain, let's get into treatment methods.
How can foot arch pain be treated?
Foot arch pain treatment can sometimes be frustrating due to our reliance on our arch. Staying off our feet to reduce stress on the arch can be challenging, but fortunately, there are several effective treatment options for foot arch pain. Depending on the intensity of the pain, you may choose a DIY treatment method. If your arch pain is persistent or severe, we recommend seeing a foot specialist to discuss treatment options and create a treatment plan.
Rest and ice
A mix of rest and ice is an effective treatment method for foot arch pain. First, temporarily reduce impactful activities and allow your feet to rest. Supplement rest with icing to keep swelling and inflammation down. (You can even use a frozen water bottle as an icy massage tool by rolling your feet on the bottle.) Then, when you feel like you're on the upswing, ease slowly back into physical activity. Avoid returning to strenuous activity to allow your body to readjust from rest to being active.
Stretching
Stretching exercises can help improve flexibility and relieve tension in the arches. Here are a few effective stretching and strengthening exercises for arch pain:
Place a towel on the floor, and grab the towel with your toes pulling it towards you.
Grasp your toes (while seated), and scrunch them towards you to feel a stretch in your arch.
Lean against a wall with your arms extended, and move your hips forward to stretch your calves.
Shockwave Therapy
This non-invasive innovative treatment delivers high-energy sound wave pulses to the affected area. Shockwave therapy triggers your body’s natural healing response to repair the damaged tissue in the arch area and reduce pain. Shockwave therapy is scientifically proven to be a highly effective treatment for chronic arch pain caused by plantar fasciitis. It is an excellent supplement to other treatments like orthotics and supportive footwear.
Orthotics
Custom-made orthotics can provide additional support and cushioning to the arches, which can help reduce pain and discomfort. Orthotics work to correct or accommodate biomechanical abnormalities, foot deformities, and other conditions to improve your gait and manage pain. The purpose of orthotics is to redistribute the force and pressure placed on our muscles and joints when we move. Equal distribution across your feet means fewer aches and pains as your muscles work better in tandem instead of select groups overworking.
Supportive footwear
Shoes with good arch support can alleviate arch pain, much like orthotics can. Wearing the proper footwear for your feet and the purpose is the least we can do for our feet. Supportive footwear acts to provide both the correct cushioning and
Physical therapy
Physical therapy can help improve strength, flexibility, and range of motion in the feet and ankles. Keeping your feet strong and balanced is vital to proper arch support. Over time, the tendons and ligaments of the arch tend to weaken. Physical therapy can help combat age and fallen arches.
Medications
You may supplement the above treatment methods with over-the-counter medication like ibuprofen or acetaminophen to reduce inflammation. Consult a doctor if you have intense pain or have questions about dosage or the recommended medication.
March 13, 2023
Arch pain is among the most common forms of foot discomfort. It can be particularly uncomfortable because of how critical the arch and heel are to the foot. The arch is the supporting foundation of our feet and appropriately resembles the shape of an aqueduct. Given the daily demands of life, it's easy to see how these structures can become overworked and damaged. The most common cause of arch pain and heel pain is a condition called plantar fasciitis.
Keep reading to learn about the most effective plantar fasciitis treatments, including shockwave therapy, custom orthotics, and pain management solutions, to help you conquer the pain of plantar fasciitis for good.
What is plantar fasciitis?
Plantar fasciitis is when you experience pain or discomfort in the heel and underside of the foot - including the arch. Inflammation or irritation of the plantar fascia, a thick band of tissue that extends between the heel bone and the arch, triggers plantar fasciitis.
Symptoms of plantar fasciitis may include:
Pain in the heel or underside of the foot. Pain may peak in the morning or after prolonged periods of standing or walking.
Stiffness and tenderness in the foot.
Swelling or redness in the foot.
Difficulty walking or standing for long periods.
What causes plantar fasciitis?
Plantar fasciitis is a common condition, especially among athletes and people who spend long periods on their feet. Understanding the source of your plantar fasciitis can help determine the best plantar fasciitis treatments for you. Causes of plantar fasciitis include:
Overuse: Repetitive activities that stress the plantar fascia, such as running, jumping, or standing for long periods, can overwork the plantar fascia, leading to inflammation and pain.
Lower leg biomechanics: Some foot structures can stress the plantar fascia and increase the risk of plantar fasciitis. Flat feet or high arches, for instance, may cause plantar fasciitis by adding stress to the muscle group.
Footwear: Improper footwear that (1) doesn't provide enough arch support, (2) doesn't have enough support or cushioning, or (3) doesn't fit properly can all contribute to plantar fasciitis.
Age: Plantar fasciitis is common in people over 40, as the plantar fascia loses elasticity and becomes more prone to injury with age.
Medical conditions: Obesity, diabetes, and osteoarthritis can increase the risk of plantar fasciitis.
Tight or weak muscles: Tight muscles in the calf or foot can put extra stress on the plantar fascia, leading to inflammation and pain.
Weight: Sudden weight gain can add stress to the plantar fascia before your body acclimatizes to the high support requirement.
The causes of plantar fasciitis can vary from person to person, and a combination of factors may contribute to the development of the condition. Consulting with a healthcare professional, such as a chiropodist, can help identify the underlying causes of your plantar fasciitis and guide appropriate treatment.
What are the effective treatment methods for plantar fasciitis?
There are many effective treatments for plantar fasciitis. Depending on the severity of the condition, you can treat the pain and discomfort yourself or be better off seeing a foot specialist. We recommend the following treatments for plantar fasciitis:
Rest
Avoiding activities that cause pain can help reduce inflammation and allow the plantar fascia to heal. Rest is the number one treatment method for plantar fasciitis as you remove the source cause. You may only need a few days of recovery, but more severe cases may need up to 4-6 weeks. After adequate rest, you may slowly resume physical activity and be on your feet.
Ice
Applying ice to the affected area can help reduce pain and swelling. You can freeze a water bottle, and rest your foot on top of it while sitting. The cold therapy reduces inflammation.
Footwear modifications
Wearing supportive shoes or inserts can help reduce stress on the plantar fascia and improve foot biomechanics. You should also remove ill-fitting footwear from your closet. Instead, choose one of our best shoes for plantar fasciitis relief.
Physical therapy
Physiotherapy and massage therapy effectively treats plantar fasciitis if you prefer not to DIY. At home, you can self-massage by rolling a tennis ball or frozen water bottle under the foot. Self-message strengthens the foot arch muscles and relieves tension in the inflamed plantar fascia.
Stretching and strengthening are also critical parts of plantar fasciitis treatment. Towel stretches, calf stretches, tennis ball rolls, and marble pickups can help strengthen the arch and heel. Find out how to effectively do plantar fasciitis exercises here.
Shockwave therapy
This non-invasive innovative treatment delivers high-energy sound wave pulses to the affected area. It triggers your body's natural healing response to repair the plantar fascia and reduce pain. Shockwave therapy is scientifically proven to be a highly effective treatment for plantar fasciitis pain persisting longer than six months.
Custom orthotics
Custom orthotics and orthopedic shoes support the arches of your feet and reduce stress on the plantar fascia. Both also encourage proper heel-to-toe gait, which, combined with arch support, can prevent a recurrence.
Taping
Taping isn't just for sports. Elastic therapeutic taping techniques may prevent unwanted movements that increase strain on the plantar fascia. For example, research finds that “in the short-term, taping is beneficial in treating plantar fasciitis. The best evidence exists for low dye taping and calcaneal taping.” Behind-the-scenes, taping provides stability and structure to the muscle group. Our chiropodists at Feet First Clinic can skillfully and therapeutically tape the feet and toes to treat and prevent a variety of foot conditions and deformities.