Small things, applied consistently and over long periods of time, lead to massive success. The opposite is also true. Small problems, if left ignored, can become significant over time. The power of time, and the external factors that affect our feet, can turn a small foot problem into a lifelong condition if not treated early.
This is only one of many important reasons why you should take good care of your feet. We’re here to help. As Toronto’s leading foot clinic, we can help address and treat foot conditions early, so they don’t impact you later in life.
Foot conditions can generally be categorized as either treatable or manageable. Treatable foot conditions are those that can go away with proper care. Examples include blisters, black toenails, athlete’s foot, smelly feet, and calluses.
Conversely, some foot conditions alter the anatomy of the foot. For the sake of simplicity, progressive foot conditions are manageable, but not truly curable. These conditions worsen over time if not treated early, and as we age, but are generally not reversible. Progressive foot conditions include bunions, bone spurs, and osteoarthritis. These type of foot conditions can worsen if you take the approach of, “oh, I’ll deal with that later,” “it’ll get better on its own,” or “it’s not that serious.”
Physical treatment can help maintain quality of life for these conditions but there is no cure like there might be for blisters or corns. That’s why it’s important to monitor foot health regularly, as these conditions can often be avoided if caught early. Alternatively, surgery is an option to remove or alter the deformity, although there are pros and cons to surgical procedures.
Below you’ll find a list of common progressive foot conditions that can worsen, and be ultimately reversible, over time if left untreated.
Bunions
Bunions are the most prevalent foot condition that can worsen over time. Up to one in three people over 18 have bunions.
Hallux rigidus

Hallux rigidus develops as a result of Osteoarthritis. The condition’s name is derived from the term “stiff big toe.”
As the metatarsophalangeal (MTP) joint breaks down, often due to repetitive use, the body responds by growing excess bone as a defence mechanism. As the area becomes increasingly crowded with this bony outgrowth, flexibility decreases in their big toe. The condition can worsen if the first long bone (metatarsal) in the forefoot begins to rub against the first bone of the big toe. The bony outgrowth known as osteophyte becomes a bone spur.
The irreversibility of this condition is due to bone presence. The only method of removing a bone spur is through surgery. With the proper physical treatment, footwear, and foot care, you can lessen the growth of a bone spur, but it will always be there.
Heel spur
Like a bone spur on the top of the foot, a heel spur is a benign bony growth on the underside of the heel bone.
- Wear supportive shoes with good shock absorption and arch support
- Avoid heels higher than 2”
- Switch to lower-impact sports
- Routinely stretch your arches, Achilles tendons, and calves
Morton’s neuroma
Morton’s Neuroma is a type of nerve compression syndrome felt as pain in the bottom of the foot. This condition affects nerves in the smaller toes.
Repetitive trauma results in fibrosis and thickening of nerve tissue, most commonly in the intermetatarsal space between the second and third toe, or the third and fourth toe. In and of itself, repetitive trauma is normal. But, poor mechanics, foot type, and footwear can over time lead to overworked areas of the foot. So, prevention is aimed at controlling these factors. To help deal with the foot’s biomechanical abnormalities, we recommend custom-made orthotics.
Osteoarthritis
Osteoarthritis is the most common form of arthritis. This is a non-inflammatory type of arthritis and a degenerative joint disease characterized by both a breakdown of cartilage and a build-up of osteophytes. The most common sites of osteoarthritis in the body is the big toe joint, followed by knees, hands and then hips.
This broad term is the common denominator in almost all the conditions you’ll find on this list. It often leads to the foot conditions you know, including bunions, bone spurs, and Morton’s neuroma. As there’s no viable replacement for joints worn down by repetitive use, the best form of action (if not caught early) is physical treatment and management. Proper shoes (specific to your needs) and custom foot orthotics can help manage pain, and prevent further deformity.
Rheumatoid arthritis
Rheumatoid Arthritis (RA) is a chronic immune mediated inflammatory disease of unknown etiology. It is the second most common form of chronic arthritis after osteoarthritis. Unlike osteoarthritis, rheumatoid arthritis affects the lining of your joints
Rheumatoid arthritis is an uncontrolled proliferation of synovial cells which erodes the surrounding bone. This erosion leads to joint damage. Damage to the tendons and ligaments can also occur, which can lead to muscle atrophy from underuse. The result is chronic pain, joint dysfunction and disability.
Currently, there is no cure for RA. However, there are many ways to effectively manage the disease’s progression, reduce stiffness and swelling, and maintain mobility in the joint.
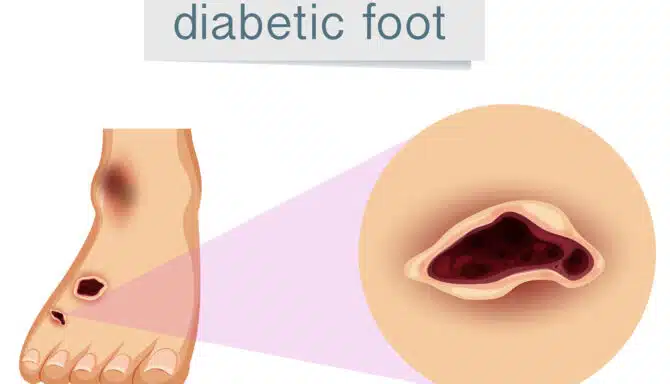
Charcot foot
Charcot foot is a rare but serious complication that can affect persons with peripheral neuropathy, especially those with diabetes. This foot condition affects the bones, joints, and soft tissues of the foot or ankle. The bones weaken, and even break, while joints in the foot or ankle can dislocate.
If not caught in its earliest stage, the joints in the foot collapse and the foot eventually becomes deformed.
Progressive Foot Conditions—Worry Not!
We pride ourselves in effectively communicating your concerns and needs as comfortable as possible. Call anytime to ask about your specific concern and we’ll make sure to provide actionable steps towards getting your feet as happy and healthy as possible!
Call us at 416-769-3338 or Book Your Assessment Today!