November 27, 2025
Your feet are essential to your mobility and independence, yet they’re commonly overlooked in everyday health routines. Proper foot care is about more than aesthetics; it helps prevent discomfort, reduce the risk of injury, and support your overall well-being.
At Feet First Clinic in Toronto, our chiropodists treat everything from nail and skin concerns to pain and mobility issues. Here are the top five ways to take care of your feet to keep them healthy and strong all year round.
1. Keep Your Feet Clean and Dry
Healthy feet start with good hygiene. Wash your feet daily with warm water and mild soap, and don’t forget to clean between the toes. After washing, dry your feet thoroughly (especially between the toes) to help prevent fungal infections like athlete’s foot.
If your feet tend to sweat a lot, moisture-wicking socks or antibacterial foot deodorant powder can help keep them dry and fresh.
2. Moisturize to Prevent Cracked Heels and Dry Skin
Dry, flaky, or cracked skin on the feet can be uncomfortable and, if left untreated, may lead to infection. Applying a foot cream or urea-based moisturizer daily helps lock in moisture and keeps the skin soft and supple.
Focus on the heels and soles, but avoid putting lotion between the toes as excess moisture there can increase the risk of fungal infections.
If you have thick, rough skin or painful calluses, a chiropodist at Feet First Clinic can safely debride (shave down) the skin and recommend medical-grade moisturizers to help prevent recurrence.
3. Trim Your Toenails Properly
Toenail care is more important than it might seem. Cutting nails too short or rounding the corners can cause ingrown toenails, which are painful and can become infected. Trim your nails straight across and gently file any sharp edges.
If your nails are thick, discoloured, or difficult to trim, don’t force it. Our chiropodists have specialized tools to safely and comfortably trim thick toenails, and we can check for signs of fungal infections or other nail concerns.
Feet First Tip: The best time to trim your toenails is after a shower when they’re softer and easier to cut.
4. Choose Proper Footwear
Your shoes play a huge role in your foot health. Wearing shoes that are too tight, narrow, or unsupportive can lead to corns, calluses, bunions, or heel pain.
When buying new shoes, make sure:
There’s about a finger’s width of space between your longest toe and the front of the shoe.
The heel fits snugly without rubbing or pressure.
You can wiggle your toes freely.
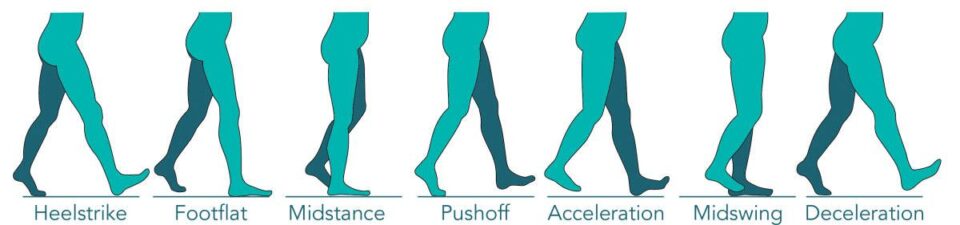
If you have foot pain, flat feet, or high arches, custom orthotics may be a game-changer. At Feet First Clinic, our chiropodists assess your gait and foot structure to design orthotics that support your body from the ground up.
5. Schedule Regular Foot Checkups
Even if your feet feel fine, regular checkups can help prevent problems before they start. Chiropodists are trained to detect and treat a wide range of foot and nail conditions, including:
Ingrown and fungal toenails
Corns, calluses, and cracked heels
Plantar fasciitis and heel pain
Diabetic foot complications
At Feet First Clinic, we believe prevention is the best medicine. Routine foot care helps maintain comfort, mobility, and confidence — especially as we age or if we spend long hours on our feet.
Feet First Tip: If you notice pain, swelling, or changes in your toenails or skin that don’t go away, it’s time to book an appointment. Small issues can quickly become big problems if ignored.
October 30, 2025
Extensor tendonitis is a common foot condition that affects the tendons running along the top of your foot. These tendons connect your muscles to your toes and help lift your toes and foot during walking and other activities. When these tendons become inflamed or irritated, it can lead to pain and difficulty moving your foot comfortably.
What Is Extensor Tendonitis?
Extensor tendonitis refers to inflammation or irritation of the extensor tendons on the top of the foot. This condition often results from overuse, repetitive strain, or injury. People who are active in sports, wear tight footwear, or have certain foot structures may be more prone to developing extensor tendonitis.
Causes of Extensor Tendonitis
Overuse: Repetitive activities such as running, jumping, or walking long distances.
Improper Footwear: Shoes that are too tight or have insufficient space on the top can compress the tendons.
Foot Mechanics: Flat feet, high arches, or gait abnormalities can put extra strain on the tendons.
Injury: Trauma or sudden impact to the foot.
Underlying Conditions: Arthritis or inflammatory diseases may contribute to tendon irritation.
Symptoms of Extensor Tendonitis
Pain and tenderness on the top of the foot, especially over the affected tendon.
Swelling or redness along the top of the foot.
Difficulty lifting the toes or foot.
Pain worsens with activity and improves with rest.
Occasionally, a burning or tingling sensation.
Treatment Options
Rest and Activity Modification
Avoid activities that aggravate the pain and allow the tendon to heal.
Proper Footwear
Wear shoes with adequate space in the toe box and good support to reduce pressure on the top of the foot.
Ice Therapy
Apply ice packs to reduce inflammation and pain.
Physical Therapy
Stretching and strengthening exercises can improve tendon flexibility and foot mechanics.
Orthotics
Custom orthotics may help correct biomechanical issues that are causing excess strain on the extensor tendon and muscles on top of the foot.
Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) can reduce pain and inflammation.
When to See a Specialist
If pain persists beyond a few weeks or worsens, consult a chiropodist or foot specialist for a biomechanical assessment and personalized treatment plan.
October 2, 2025
The Achilles tendon is the strongest tendon in the body. It connects your calf muscles to your heel bone and enables activities like walking, running, and jumping. However, it is also prone to injury -particularly from overuse. Two common conditions affecting the Achilles tendon are Achilles tendonitis and Achilles tendinosis. Although their names sound similar, they differ in causes, symptoms, and treatment approaches. Understanding these differences is crucial for effective recovery and prevention.
What Is Achilles Tendonitis?
Achilles tendonitis is an acute inflammation of the Achilles tendon, typically caused by sudden increased activity or repetitive strain. It results in swelling, pain, and irritation along the tendon.
Typical pain in a male jogger`s achilles tendon. XXL size image.
Causes of Achilles Tendonitis:
Sudden increase in physical activity or intensity
Overuse during running or jumping sports
Poor footwear
Training on hard surfaces
Tight calf muscles
Poor biomechanics
Symptoms of Achilles Tendonitis:
Sharp or burning pain along the back of the heel or lower calf
Swelling and tenderness over the tendon
Stiffness, especially in the morning or after rest
Pain worsens with activity
What Is Achilles Tendinosis?
Achilles tendinosis is a chronic condition characterized by degeneration of the tendon’s collagen fibers without significant inflammation. It often develops after untreated or recurrent Achilles tendonitis and results in thickening and weakening of the tendon. It's essentially what can happen if Achilles tendonitis goes untreated.
Causes of Achilles Tendinosis:
Repeated micro-tears and poor healing
Chronic overuse without adequate rest
Aging and reduced blood supply to the tendon
Biomechanical abnormalities
Symptoms of Achilles Tendinosis:
Dull, persistent pain along the tendon
Thickened or nodular tendon
Decreased strength and flexibility in the calf and ankle
Pain may improve with warm-up but worsen with prolonged activity
Key Differences Between Tendonitis and Tendinosis
FeatureAchilles TendonitisAchilles TendInosisNatureInflammatoryDegenerative (non-inflammatory)DurationAcute or subacuteChronic, long-termTissue ConditionInflamed tendon fibersDegenerated, disorganized fibersPainSharp, localizedDull, diffuseTreatment FocusReduce inflammation, restPromote tendon healing, strengthen
Treatment Options
For Achilles Tendonitis:
Rest and activity modification
Ice and anti-inflammatory medications
Physical therapy focusing on stretching and strengthening
Proper footwear and orthotics
Gradual return to activity
For Achilles Tendinosis:
Eccentric strengthening exercises to stimulate tendon repair
Physical therapy and stretching
Shockwave therapy or ultrasound treatments
Possible use of platelet-rich plasma (PRP) injections
Surgery in severe, unresponsive cases
Prevention Tips
Warm up properly before exercise
Gradually increase activity intensity and duration
Wear supportive, well-fitting shoes
Maintain calf flexibility and strength
Avoid running on hard or uneven surfaces when possible
July 10, 2025
What is an Ankle Foot Orthotic (AFO)?
An ankle foot orthotic (AFO) is a medical-grade brace that supports the foot and ankle. It often extends partway up the calf. Unlike regular foot orthotics—which fit inside shoes to support the arch and heel. AFOs offer external stabilization of both the foot and ankle joints.
AFOs are commonly made of lightweight plastic or carbon fiber and may be custom-made or prefabricated. They assist walking, correct alignment, reduce pain, and help prevent further injury.
Who Needs an AFO?
Image from https://braceworks.ca/ and the Washington Post
AFO's received mainstream attention a few years ago when NFL quarterback Alex Smith returned to the football field after a catastrophic leg injury. The key to his return: an ankle foot orthotic. Due to a post-surgical infection, the nerve that helps flex the right foot was severed. This meant he couldn't lift his foot. So he got an AFO to help and made a brief comeback (with the help of an extensive rehab team).
So who exactly needs an AFO? Since AFOs are heftier than regular orthotics, they're typically recommended for patients with more complex conditions than those addressed by traditional foot orthotics. You might benefit from an AFO brace if you have:
Foot drop (difficulty lifting the front of the foot)
Cerebral palsy or neuromuscular disorders
Stroke-related gait issues
Multiple sclerosis (MS)
Post-surgical ankle instability
Tendon or ligament injuries
Severe arthritis affecting ankle mechanics
Ankle foot orthotics are most commonly indicated for neuromuscular disorders and foot drop.
AFOs v Regular Orthotics: What's the Difference?
FeatureRegular OrthoticsAnkle Foot Orthotics (AFOs)ScopeFoot support onlyFoot and ankle supportPlacementInside the shoe (underneath the foot)Worn underneath and around the foot, and around the ankleConditions TreatedArch pain, plantar fasciitis, overpronation, high arches, other biomechanical irregularitiesNeurological and structural gait disorders, severe instabilityCustomizationOften custom-fit or prefabOften custom-molded to leg shapeMobility SupportModerateHigh—can aid in walking and balance
While regular orthotics focus on redistributing pressure and correcting foot mechanics inside the shoe, AFOs provide external control for more complex biomechanical or neurological issues. Think of it as the difference between cushioning a sore spot and physically guiding your limb’s motion.
How Are AFOs Made and Fitted?
https://www.youtube.com/watch?v=nA_QklH7AWY
AFOs are usually prescribed by a foot specialist or chiropodist after a full assessment. The process may include:
Biomechanical Assessment
Gait analysis
Casting or 3D scanning
Custom fabrication
Fitting and adjustments
Some patients may only need short-term use post-injury or surgery, while others may rely on AFOs for long-term mobility support.
Final Thoughts
If you’ve been told you need more than just arch support or if your walking pattern has changed due to injury or illness, an ankle foot orthotic could be a game-changer. At our clinic, we assess your full biomechanics and work with you to find the right support—whether that’s a custom orthotic, AFO, or a combination of both.
June 12, 2025
When we talk about healthy habits, we often focus on nutrition, mental health, or overall fitness. But what about your feet? These often-overlooked heroes carry you through life and they deserve some attention, too.
Incorporating a few gentle foot mobility drills into your morning routine can help improve flexibility, reduce stiffness, and set you up for a pain-free day. Let’s explore a few simple daily foot exercises that support longevity and mobility, all in under 10 minutes.
Why Morning Foot Rituals Matter
After a night of rest, it’s normal for your feet to feel stiff or tight. That’s because circulation slows down when we sleep, and our muscles and joints aren’t being used. A quick morning routine for foot health helps:
Improve blood flow
Gently wake up foot muscles
Prevent long-term issues like plantar fasciitis or joint stiffness
Support better balance and stability throughout the day
Plus, it feels great — and your feet will thank you!
Your 5-Minute Morning Routine for Foot Health
These beginner-friendly exercises can be done from your bed, the bathroom counter, or even while you’re waiting for your coffee to brew.
1. Toe Spreads (1 minute)
https://youtube.com/shorts/gOwgyrmU6hM?feature=shared
Sit or stand comfortably. Spread your toes apart as wide as you can, then release. Repeat 10–15 times.Why it helps: Improves foot strength and activates the smaller intrinsic foot muscles that support balance.
2. Ankle Circles (1 minute per foot)
https://youtu.be/qaatVpZy2ek?feature=shared
Lift one foot off the ground and gently rotate your ankle clockwise 10 times, then counter-clockwise 10 times. Switch feet.Why it helps: Promotes circulation and joint mobility to counteract morning stiffness.
3. Towel Curls (1–2 minutes)
https://youtu.be/toqnSys_JRw?feature=shared
Place a small towel on the floor and try to scrunch it toward you using just your toes.Why it helps: Strengthens the arches and enhances coordination in the foot muscles.
4. Calf Stretch with Wall or Step (1–2 minutes)
https://youtu.be/utLavyPDnqI?feature=shared
Stand with your hands on a wall or place your toes on a step while your heel stays on the ground. Lean forward until you feel a stretch in your calf and Achilles tendon. Hold for 20–30 seconds per leg.Why it helps: Loosens up the back of the leg and heel — essential for preventing plantar fasciitis and Achilles tendonitis.
Bonus: Gentle Foot Massage
https://youtu.be/BwhGFoHDkUI?feature=shared
Before putting on your socks or shoes, use your thumbs or a massage ball to roll out the soles of your feet. Focus on tight spots in the arch and heel. Just 1–2 minutes can make a big difference.
Foot Mobility Drills = Long-Term Foot Wellness
Incorporating these foot mobility drills into your morning can support not just your feet, but your entire body. Improved foot function leads to better posture, less knee and hip pain, and more stability with every step you take.
And remember — consistency is key. Like any good habit, the benefits of daily foot exercises build up over time.
Feature Photo by Aljona Ovtšinnikova
May 29, 2025
When you think of dehydration, you probably imagine symptoms like dry mouth, fatigue, or dizziness, but what about your feet? It may surprise you to learn that dehydration can directly contribute to foot pain, cramping, and even swelling. Since your feet are at the farthest point from your heart, they rely heavily on healthy circulation and fluid balance to function properly.
Let’s take a look at how your water intake affects your fee and why staying hydrated is more important than you might think.
1. Dehydration and Foot Cramps
If you’ve ever woken up in the middle of the night with a painful foot cramp, dehydration might be the culprit. Proper hydration is essential for normal muscle function. Without enough fluids, your muscle (especially in your feet and calves) can tighten up unexpectedly.
Cramps often occur when your body is low on essential electrolytes like potassium, magnesium, and sodium, which are lost through sweat. Since water helps regulate these minerals, not drinking enough can increase your risk of sudden, painful cramps in the feet.
2. Hydration Supports Circulation in the Feet
Good circulation is critical for healthy feet. Water plays a major role in keeping your blood flowing efficiently. When you’re dehydrated, your blood volume decreases, making it harder for your heart to pump blood to the extremities—including your feet.
Poor circulation can lead to sensations of numbness, tingling, or a “pins and needles” feeling in your feet. In more severe cases, chronic dehydration could contribute to long-term circulatory problems that make foot pain worse over time.
3. Water Helps Lubricate Joints and Reduce Pain
Your feet contain more than 30 joints, all of which rely on synovial fluid for smooth, pain-free movement. Dehydration reduces your body’s ability to produce this fluid, leading to stiff, achy joints—especially in people with arthritis or other joint conditions.
Drinking enough water each day can help reduce joint discomfort and improve mobility in your feet and ankles.
4. Is Water Retention the Opposite Problem?
Interestingly, dehydration can also lead to swollen feet—but not for the reason you might think. When your body senses it's not getting enough water, it holds onto the fluids it does have. This can result in swelling (also known as water retention) in the feet, ankles, and lower legs.
Staying properly hydrated signals your body that it can safely release excess fluids, helping to reduce swelling and bloating in the feet.
5. Tips to Keep Your Feet (and the Rest of You) Hydrated
Aim for 8–10 glasses of water per day, and more if you're physically active or it's hot outside.
Avoid too much caffeine or alcohol, as these can dehydrate your body.
Eat water-rich foods like cucumbers, oranges, and watermelon.
Listen to your body—if you're feeling thirsty, you're likely already slightly dehydrated.
When to Seek Help
If you’re experiencing regular foot pain, cramping, or swelling—especially if increasing your water intake doesn’t help—it’s time to speak with a foot care specialist. At Feet First Clinic, our chiropodists can assess the cause of your symptoms and recommend personalized treatment options to get you back on your feet comfortably.
Final Thoughts
Dehydration doesn’t just leave you feeling tired—it can seriously impact your foot health. From muscle cramps to water retention, the way you hydrate has a direct effect on how your feet feel and function.
So next time your feet are aching or swollen, take a moment to consider your water intake. A simple increase in hydration might be the first step toward relief.